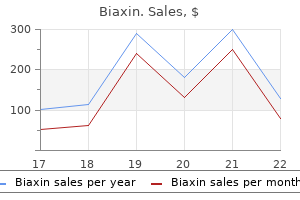
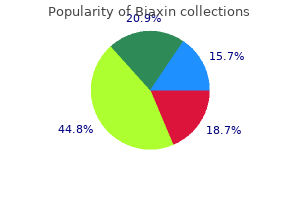
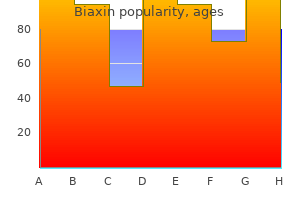
Biaxin
Biaxin dosages: 500 mg, 250 mg
Biaxin packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills

Discount 500 mg biaxin with amex
I would then apply a large pelvic discount clamp across the articular block to cut back the condylar width and compress the articular fracture strains gastritis xantomatosa biaxin 500 mg online buy cheap. On completion of this step I would launch the tourniquet and apply my round fixator gastritis diet sweet potato biaxin 500 mg generic visa. I would use a ring slightly below the articular screws and a double ring block within the tibial diaphysis, permitting me to restore the axis of the tibia. If the knee was unstable after this (on examination underneath anaesthesia), I would cross the knee with the ring fixator and plan to remove the femoral ring at 6�8 weeks. Rademakers and colleagues studied 109 patients for post-traumatic arthritis from tibial plateau fractures over 5�2 years: if good alignment was achieved, the incidence of osteosrthritis was 9% (versus 27% if the axis deviation is >5�). Weigel and Marsh looked at consequence of high-grade injuries and found a low rate of symptomatic joint arthrosis even if there was some articular incongruity. The need for meniscal resection will improve the risk of arthrosis, as will instability from cruciate dysfunction. Operative remedy of 109 tibial plateau fractures: five to 27-yr follow-up outcomes. High-energy fractures of the tibial plateau: knee function after longer follow-up. This is a closed damage with no gross neurovascular considerations however important delicate tissue harm. There is a posh, intra-articular, multifragmentary fracture extending proximally into the metaphysis. I would take full historical past and examination, concentrating on important risk elements, for instance smoking, diabetes, and peripheral vascular disease. Examination would assess gentle tissue integrity and neurovascular status with full documentation. This harm requires discount and skeletal stabilization to enable resolution of soppy tissue before definitive fixation. Once soft tissues have recovered I would think about definitive fixation depending upon the fracture configuration. This is the staged management protocol described by Sirkin, and represents the gold normal management algorithm for complicated intra-articular fractures of the tibial plafond. The scan improves recognition of fracture fragments as described by Topiliss, and helps in planning incisions to decrease further trauma to soft tissues and keep their viability. There are many alternatives, including fixation in calcaneus and talus, supplemental first metatarsal fixation to avoid equinus problems, quadrilateral body, hybrid frames, and nice wire frames. The rules are anatomical reduction and rigid fixation of the articular components, and restoration of size, alignment, and rotation of the meta-diaphyseal components, so as to restore anatomy and performance. After the preliminary success of R�edi and Allg�wer and their ideas of fixation the complication fee rose significantly within the palms of non-experts. Multiple research reported excessive complication charges (30% non-union, malunion, infection). However, the proof is starting to suggest that in appropriate centres with experienced surgeons and appropriate strategies (staged, early intervention, limited reduction) the complication price is enhancing, with excellent medical outcomes (2. Decisions and staging resulting in definitive open administration of pilon fractures: the place have we come from and the place are we now Answers these are anteroposterior and lateral views of a skeletally mature left ankle. The fibular is a spiral fracture starting on the degree of, and lengthening under the level of, the syndesmosis and the medial side is a transverse fracture. This harm wants immediate reduction within the emergency division underneath applicable analgesia or sedation to stop compromise of the medial side. I would stabilize the discount in a below-knee plaster of Paris forged, obtain radiographs to confirm sufficient discount, and organize admission for definitive fixation. There are a quantity of classifications for ankle factures primarily based on both the mechanism (Lauge-Hansen) or anatomical description (Weber) of the damage. The Weber classification pertains to the fibular with kind A beneath the syndesmosis, sort B at the stage of the syndesmosis, and sort C above. A extra detailed system is that proposed by Lauge-Hansen based upon cadaveric work. The first term represents the position of the foot and the second to the drive placed upon the foot and talus in the ankle mortise. Dorsiflexion patterns are also described and relate more to Pilon fractures than ankle accidents. The supination�adduction sample tends to have a vertical orientation to the medial malleolus and pronation�abduction tends to have a fibular fracture above the syndesmosis and a transverse or quick indirect fibular fracture due to the bending force. The absence of ache and tenderness on the medial facet is a poor indicator of the integrity of these buildings. The gravity stress view has been developed to assist affirm the integrity of the deltoid, with a medial clear space of more than 5 mm being suggestive of medial injury. Given no contraindications to surgery, my definitive administration could be operative. Using a tourniquet, and with antibiotic prophylaxis, I would fix the posterior malleolus and the lateral side although a posterolateral strategy. The posterior fixation can be a buttress plate and extra screw, with an anti-glide plate plus supplementary interfragmentary screws for the fibula. I would tackle the medial side ideally using two short (40 mm) partially threaded cancellous screws. I would defend the gentle tissues in plaster of Paris for two weeks after which begin protected weight-bearing for an extra 4 weeks. My indications for operative intervention are that this fracture can be very troublesome to preserve in place in plaster of Paris as a outcome of instability, and for a shift of greater than 1 mm in touch area the forces in the ankle joint change significantly, predisposing to post-traumatic osteoarthritis. Stress views might over-diagnose accidents and partial tears of the deep deltoid might end in positive stress views, however could possibly be successfully handled non-operatively. Evaluation of the integrity of the deltoid ligament in supination exterior rotation ankle fractures: a scientific evaluation of the literature. Does a constructive ankle stress take a look at point out the need for operative therapy after lateral malleolus fracture These anteroposterior views of the left decrease limb show a proximal third spiral fibula fracture, and an ankle mortise with widening of the medial and superior clear areas resulting in significant talar shift. This harm is a Weber type C fibular injury with associated deltoid and syndesmotic ligament ruptures. The harm pattern is unstable, and subsequently in all however extremely unfit sufferers surgical fixation would be my most popular management. In this instance, under tourniquet and image management, and with a sandbag beneath the ipsilateral buttock, I would attempt closed discount of the syndesmosis utilizing a big pelvic reduction clamp between the malleoli.
Buy 250 mg biaxin amex
The adjoining sternocleidom astoid region and the anterior cervical area are also exposed gastritis zantac biaxin 250 mg discount fast delivery. The pores and skin and subcutaneous fat have been rem oved to show the subcutaneous gastritis diet questions 500 mg biaxin buy with mastercard, purely sensory cutaneous nerves from the cervical plexus in the lateral cervical region. Speci cally these nerves are the lesser occipital, nice auricular, transverse cervical, and supraclavicular nn. Note: the transverse cervical nerve passes beneath the external jugular vein and form s an anastom osis with the cervical department of the facial nerve. This m ixed loop incorporates m otor bers from the facial nerve and sensory bers for the neck from the transverse cervical nerve. The investing layer of the deep cervical fascia has been rem oved over the posterior cervical triangle to expose the prevertebral layer of the cervical fascia, which is fused to the pretracheal lam ina on the degree of om ohyoid m uscle (see p. Note the external branch of the accessory nerve, which passes to the trapezius m uscle. This injury restricts the m obilit y of the scapula, and the affected person m ay be unable to elevate the upper lim b past 90�. In this dissection, the pretracheal layer of the deep cervical fascia has additionally been rem oved to show the om ohyoid m uscle, which is enveloped by that fascia. Note the phrenic nerve, which runs obliquely over the scalenus anterior m uscle to the thoracic inlet. The sternal end of the clavicle, the anterior end of the rst rib, the m anubrium sterni, and the thyroid gland have been rem oved to expose the thoracic inlet. Note the course of the following buildings: the interior thoracic artery descends parallel to the sternum. In patient s with coronary coronary heart disease, the interior thoracic artery could be m obilized and anastom osed to the coronary artery previous the point of the stenosis. The sympathetic trunk, vagus nerve, phrenic nerve, and portions of the brachial plexus are seen, the lat ter passing by way of the interscalene house (see C). Note also the time period ination of the thoracic duct at the jugulosubclavian venous junction and the left recurrent laryngeal nerve. This department of the vagus nerve winds around the aortic arch and ascends to the larynx. It is bounded by the sternocleidom astoid m uscle, the posterior stomach of the digastric m uscle, and the superior belly of the om ohyoid m uscle. The subm andibular gland could be seen at the inferior border of the m andible and the sternocleidom astoid m uscle has been retracted posterolaterally. The sternocleidom astoid region and carotid triangle have been dissected together with adjoining parts of the posterior and anterior cervical triangles. The carotid sheath has been rem oved on this dissection along with the cervical fasciae, sternocleidom astoid m uscle, and om ohyoid m uscle to dem onstrate all important neurovascular constructions in the neck: � Com m on carotid artery with it s division into the interior and exterior carotid arteries � Superior and inferior thyroid arteries � Internal jugular vein � Deep cervical lymph nodes alongside the interior jugular vein � Sympathetic trunk together with it s ganglia � � � � � Vagus nerve Hypoglossal nerve Accessory nerve Brachial plexus Phrenic nerve the phrenic nerve originates from the C3�C5 segm ent s and therefore is part of the cervical plexus. The m uscular landm ark for locating the phrenic nerve is the scalenus anterior, alongside which the nerve descends in the neck. The (posterior) interscalene space is situated bet ween the scalenus anterior and m edius and the rst rib and is traversed by the brachial plexus and subclavian artery. The subclavian vein passes deeply through the interval form ed by the scalenus anterior, the sternocleidom astoid m uscle (resected), and the rst rib (the anterior interscalene space). The principal arterial vessel on this region is the occipital artery, the second department arising from the posterior aspect of the external carotid artery. The m edially located higher occipital nerve is a dorsal ram us of the C2 spinal nerve, whereas the laterally located lesser occipit al nerve is a ventral ram us of C2 that arises from the cervical plexus (see p. The lym ph nodes are positioned on the sites where the nerves and veins em erge through the cervical fascia. Note the accent nerve, which crosses the lat-eral cervical triangle at a comparatively tremendous cial level. Topographical Anatomy Occipital artery Splenius capitis Sternocleidom astoid Sem ispinalis capitis Obliquus capitis superior Rectus capitis posterior m inor Greater occipital nerve Vertebral artery Rectus capitis posterior m ajor Obliquus capitis inferior Spinous process, axis (C2) Third occipital nerve Sem ispinalis cervicis m uscle Splenius capitis Suboccipital nerve Occipital artery Great auricular nerve Transverse process of atlas (C1) Cervical posterior intertransversarius Longissim us capitis Sem ispinalis capitis B Right suboccipital triang le Posterior view. The suboccipital triangle is bounded superiorly by the rectus capitis posterior m ajor, laterally by the obliquus capitis superior, and inferiorly by the obliquus capitis inferior. This m uscular triangle could be seen solely after the trapezius, splenius capitis, and sem ispinalis capitis m uscles have been rem oved. A brief, free segm ent of the vertebral artery runs through the deep part of the triangle after leaving the transverse foram en and before exiting the triangle by perforating the atlanto-occipital m em brane (not seen here). That segm ent of the vertebral artery gives o branches to the surrounding short nuchal m uscles. The exam iner take a look at s the feeling of those nerves by pressing flippantly on the circled point s with the thum b. If these point s (but not their surroundings) are painful, the nding is described, logically, as "tenderness over the occipital nerves. The pat tern of segm ental innervation is illustrated on the left, and the territorial assignm ents of speci c cutaneous nerves on the proper. The occiput and neck derive m ost of their segm ental innervation from the second and third cervical segm ent s. Note that in the peripheral innervation pat tern, the greater occipitalnerve is a dorsal spinal nerve ram us whereas the lesser occipital nerve is a ventral ram us (see p. This section of the skull may be roughly subdivided into 4 areas: the oral cavit y, the nasal cavit y and sinus, the orbit, and the anterior cranial fossa. Inspecting the area in and across the oral cavity, we observe the m uscles of the oral oor, the apex of the tongue, the neurovascular buildings within the m andibular canal, and the rst m olar. The onerous palate separates the oral cavit y from the nasal cavity, which is split into left and proper halves by the nasal septum. The inferior and m iddle nasal conchae may be identi ed together with the laterally situated m axillary sinus. The section passes by way of the transparent vitreous physique, and three of the six extraocular m uscles could be identi ed within the retro-orbital fats. Note: the bony orbital plate (m edial wall of the orbit) could be very thin (lam ina papyracea) and m ay be penetrated by infection, traum a, and neoplasm s. In the anterior cranial fossa, the part passes through both frontal lobes of the brain in the m ost anterior portions of the cerebral grey m at ter. In addition to the oral oor m uscles, we see the m uscles of m astication on the edges of the skull. The orbit com m unicates laterally with the infratemporal fossa by way of the inferior orbital ssure. This section cut s through both olfactory bulbs within the anterior cranial fossa, and the superior sagit tal sinus can be acknowledged in the m idline. The taste bud replaces the exhausting palate on this plane of part, and the nasal septum becom es osseous at this degree. This coronal part is slightly angled, producing an obvious discontinuit y within the m andibular ram us on the left facet of the gure (compare with the continuous ram us on the proper side). Above the roof of the sphenoid sinuses is the hypophysis (pituitary), which lies in the hypophyseal fossa. In the cranial cavit y, the aircraft of part passes via the m iddle cranial fossa. Due to the presence of the carotid siphon (a 180� bend within the cavernous a part of the internal carotid artery), the part minimize s the interior carotid artery t wice on each side.
Buy generic biaxin 250 mg on line
In an effort to improve footprint restoration and biomechanical strength gastritis recovery discount 500 mg biaxin with amex, repairs transitioned from a nonlinked double-row repair to a suturebridging double-row restore gastritis from stress order biaxin 250 mg on-line. Biomechanically, the aim of a rotator cuff repair is to achieve high initial fixation power, minimize gap formation, and maximize footprint contact area. In different words, whereas biology performs an essential function in rotator cuff tendon therapeutic, these biomechanical factors should be optimized by the surgeon at time 0 to present the best chance for tendon therapeutic. The conventional double-row restore consisted of unbiased rows of medial and lateral anchors during which the medial sutures had been placed in a mattress configuration and the lateral sutures had been placed as easy sutures. Suture-bridging repairs have improved footprint contact area and stress in addition to final load to failure in comparison with traditional double-row repairs. H1, thickness of rotator cuff earlier than loading; L1, length of tendon beneath suture. H2, thickness of compressed rotator cuff underneath tensile load; L2, length of tendon beneath suture; a, length of suture between tendon edge and lateral anchor; T, tensile loading force. Inset: Free-body diagram exhibiting regular force (N) distribution ensuing from elastic deformation of tendon beneath the suture. Additionally, a medial double-mattress stitch on this case supplies a seal to joint fluid. For tears bigger than 3 cm, the re-tear price increased to 45% following single-row restore vs 26% following double-row repair. These improved healing rates are necessary given that a healed rotator cuff restore is associated with a superior functional outcome at mid- and long-term follow-up. Denard et al, for instance, demonstrated that a traditional double-row restore of a massive tear was four. Frank et al reported an 88% fee of therapeutic in 25 rotator cuff tears repaired with a suture-bridging construct. Dedicated outflow is averted in order to lower turbulence since this only hinders visualization. The majority of suture passage is performed with a self-retrieving antegrade suture passer (Scorpion FastPass [Arthrex, Inc]), though a retrograde device (Penetrator [Arthrex]) is commonly helpful for suture passage via the posterior side of the rotator cuff. A towel is placed in the contralateral axilla and pillows are positioned beneath the contralateral leg as nicely as between the legs. The arm is positioned in 20 levels of flexion and 20 to 30 levels of abduction with 5 to 10 lbs of balanced suspension utilized (Star Sleeve Traction System [Arthrex]). Portal placement is important to provide an optimum angle of approach to the goal tissues, and for that purpose, aside from the preliminary posterior portal, an 18-gauge spinal needle is used to exactly establish all portals in an outside-in trend. An anterosuperolateral portal is also required for biceps tenodesis and may replace the anterior portal for diagnostic functions. For occasion, the authors sometimes place anchors via small percutaneous incisions simply lateral to the acromion to achieve the correct "deadman" angle for the suture anchors. Right shoulder posterior subacromial viewing portal demonstrates a crescent-shaped rotator cuff tear amenable to a double-row rotator cuff restore. The frequent portals are as follows: Posterior portal: the authors establish a posterior portal by palpating the delicate spot of the glenohumeral joint and enter the joint at or just below the equator of the humeral head. The actual position varies from patient to affected person however is roughly 4 cm inferior and 4 cm medial to the posterolateral nook of the acromion. This portal entry is used for the preliminary glenohumeral arthroscopy and dealing in the subacromial house. Anterior portal: this is established using an outside-in approach just superior to the lateral half of the subscapularis tendon for use during diagnostic glenohumeral arthroscopy. Lateral subacromial portal: Entry is approximately four cm lateral to the lateral side of the acromion, according to the posterior border of the clavicle. Anterosuperolateral portal: this portal is helpful for a subscapularis repair or biceps tenodesis. It is established by way of the rotator interval just anterior to the supraspinatus tendon and directly above the lengthy head of the biceps. The level of entry is roughly 1 to 2 cm lateral to the anterolateral corner of the acromion. Placement must be parallel to the subscapularis tendon and permit a 5- to 10-degree angle of approach to the lesser tuberosity. Step-by-Step Description of the Procedure When adequate tendon mobility is current, the authors carry out a suture-bridging restore of medium-sized crescent tears. When the quality of the tissue is good, the authors use a knotless SpeedBridge approach (Arthrex) with FiberTape (Arthrex) and 2 rows of BioComposite SwiveLock C suture anchors (Arthrex). The steps for a SutureBridge repair are basically the identical, with the exception that more suture passes are performed medially and all sutures are tied earlier than linking the sutures to the lateral row. Prepare the Soft Tissues and Bone Bed Following a diagnostic arthroscopy and completion of intra-articular and/or subscapularis work, the delicate tissues and greater tuberosity bone mattress are prepared. A bursectomy is completed and allows the surgeon to see the whole margin of the cuff tear. Any bursal leaders that attach to the internal deltoid fascia are debrided in order that the tendon edge is clearly seen. Soft tissue is removed from the greater tuberosity with an electrocautery device and a highspeed burr is used to frivolously "mud off the charcoal. Medial Anchor Placement A spinal needle identifies the right method from the lateral acromial boarder to the medial side of the footprint. A punch is then inserted via a percutaneous incision and used to create a bone socket for a SwiveLock C suture anchor. A SwiveLock anchor preloaded with FiberTape suture is placed through the same percutaneous portal used for punch insertion. Once the motive force tip is fully inserted into the ready bone gap, the screw is delivered. The insertion sheath is backed off to affirm that the highest of the anchor is seated at or just under the bone floor. Suture Passage It is necessary to restore the traditional length-tension relationship of the tendon. The location of medial suture placement is crucial and can determine the medial-to-lateral pressure. The authors consider that such medial placement is largely liable for the stories of medial tendon failure following double-row restore. A grasper may be used to scale back the tendon in order that the surgeon can establish the ideal location for placement of the medial sutures, often 2 to three mm lateral to the musculotendinous junction. Once the medial-tolateral location is set, the anterior-to-posterior suture placement is evenly spaced relative to the anchor. For the SpeedBridge repair, all sutures from a medial anchor are handed through the rotator cuff first. The FiberTape sutures can simply be passed by way of the rotator cuff with an antegrade suture passer (Scorpion) and retrieved. In the SutureBridge package, the 2 ends of the FiberWire are delivered collectively so that each FiberTape sutures limbs can be passed by way of the rotator cuff in a single move. However, in most cases, the authors choose to also cross the eyelet security sutures through the identical location so that a medial double-pulley restore can additionally be carried out. This step is achieved with a FiberLink suture, which is used to shuttle the FiberTape and the FiberWire eyelet sutures via the rotator cuff.
Best biaxin 500 mg
The super cial m iddle cerebral vein drains into both the cavernous and transverse sinuses (see A gastritis special diet cheap 250 mg biaxin mastercard, p gastritis zofran buy 250 mg biaxin with mastercard. Olfactory nerve Anterior com m unicating vein Optic tract Interpeduncular vein Inferior choroidal vein Basilar vein Superficial m iddle cerebral vein Anterior cerebral vein Deep m iddle cerebral vein Cerebral peduncle Internal cerebral vein Great cerebral vein Posterior venous confluence C Basal cerebral venous system the basal cerebral venous system drains blood from each super cial and deep cerebral veins. A venous circle kind ed by the basilar veins (of Rosenthal, see below) exist s at the base of the mind, analogous to the arterial circle of Willis. The basilar vein is kind ed within the anterior perforate substance by the union of the anterior cerebral and deep m iddle cerebral veins. Following the course of the optic tract, the basilar vein runs posteriorly around the cerebral peduncle and unites with the basilar vein from the opposite aspect on the dorsal side of the mesencephalon. The t wo internal cerebral veins additionally term inate at this venous junction, the posterior venous con uence. This junction provides rise to the m idline great cerebral vein, which enters the straight sinus. The t wo anterior cerebral veins are interconnected by the anterior com m unicating vein, making a closed, ringshaped drainage system. Superior sagit tal sinus Superficial cerebral veins Medullary anastom otic vein Superficial cerebral veins Medullary vein Longitudinal vein of caudate nucleus Transverse veins of caudate nucleus Choroidal vein Internal cerebral vein Term inal vein Deep m iddle cerebral vein Inferior lenticular veins Vein of centrum sem iovale Superficial m iddle cerebral vein Lateral superior lenticular veins Medial superior lenticular veins D Anastomoses betw een the super cial and deep cerebral veins Transverse part by way of the left hem isphere, anterior view. The tremendous cial cerebral veins com m unicate with the deep cerebral veins by way of the anastom oses proven here (see p. Flow reversal (double arrows) might occur in the boundary zones guess ween t wo territories. The temporal and occipital lobes and tentorium cerebelli have been rem oved on the left side to dem onstrate the upper floor of the cerebellum and the superior cerebellar veins. On the lateral walls of the anterior horns of both lateral ventricles, the superior thalam ostriate vein runs toward the interventricular foram en within the groove bet ween the thalam us and caudate nucleus. After receiving the anterior vein of the septum pellucidum and the superior choroidal vein, it type s the internal cerebral vein and passes through the interventricular foram en alongside the roof of the diencephalon towards the quadrigem inal plate, which incorporates the superior and inferior colliculi. There it unites with the internal cerebral vein of the other aspect, and the basal veins to form the posterior venous con uence, which gives rise to the nice cerebral vein. Veins of caudate nucleus Anterior vein of septum pellucidum Internal cerebral vein Basal vein Posterior vein of corpus callosum Interventricular foram en Superior thalam ostriate vein Superior choroidal vein Lateral vein of lateral ventricle Great cerebral vein Medial vein of lateral ventricle Straight sinus Superior cerebellar veins Confluence of the sinuses Quadrigem inal plate Inferior petrosal sinus Petrosal vein Sigm oid sinus Great cerebral vein Superior vein of verm is Superior petrosal sinus Verm is (Lateral) inferior cerebellar vein (Lateral) superior cerebellar vein (Medial) superior cerebellar vein Transverse sinus Straight sinus (Medial) inferior cerebellar vein Confluence of the sinuses Inferior vein of verm is B Cerebellar veins Posterior view. Like the other veins of the brain, the cerebellar veins are distributed independently of the cerebellar arteries. Larger trunks cross over gyri and sulci, running m ainly in the sagit tal direction. A medial and a lateral group may be distinguished based mostly on their gross topographical anatomy. The m edial group of cerebellar veins drains the verm is and adjacent parts of the cerebellar hem ispheres (precentral vein, superior and inferior veins of the verm is) and the m edial parts of the superior and inferior cerebellar veins. The lateral group (petrosal vein and lateral portions of the superior and inferior cerebellar veins) drains m ost of the t wo cerebellar hem ispheres. All of the cerebellar veins anastom ose with one another; their out ow is solely infratentorial. Blood Vessels of the Bra in Internal cerebral vein Inferior sagit tal sinus Thalam ostriate vein Anterom edial anastom osis Anterolateral anastom osis Trigem inal nerve Anterom edian pontine vein Transverse pontine veins Interpeduncular veins Pontom esencephalic vein Superior verm ian vein Superior cerebellar veins Anterolateral pontine vein Basal vein C Reg ion drained by the deep cerebral veins Coronal part. Three principal venous segm ents may be identi ed in every hem isphere: � Thalam ostriate vein � Internal cerebral vein � Basal vein the area drained by the deep cerebral veins encompasses giant parts of the bottom of the cerebrum, the basal ganglia, the internal capsule, the choroid plexuses of the lateral and third ventricles, the corpus callosum, and parts of the diencephalon and m esencephalon. Transverse m edullary veins a Posterom edian m edullary vein Posterior choroidal vein Internal cerebral veins D Veins of the brainstem a Anterior view of the brainstem in situ (the cerebellum and part of the occipital lobe have been rem oved on the left side). The veins of the brainstem are a continuation of the veins of the spinal wire and connect them with the basal veins of the brain. The veins of the m edulla oblongata, pons, and cerebellum m ake up the infratentorial venous system. Great cerebral vein Superior cerebellar vein Trigem inal nerve Superior petrosal vein Accessory basal vein Trochlear nerve Variant of basal vein Lateral m esencephalic vein Lateral m edullary vein Posterolateral medullary vein Dorsal transverse m edullary veins b Posterom edian m edullary vein Caudal cerebellar peduncular vein Vein of cerebellom edullary cistern 379 Neuroanatomy 17. A Extracerebral hemorrhages Extracerebral hem orrhages are de ned as bleeding guess ween the calvaria and brain. Because the bony calvaria is im m obile, the creating hem atom a exert s strain on the soft mind. Depending on the source of the hem orrhage (arterial or venous), this m ay produce a quickly or slowly creating incompressible m ass with a rise of intracranial pressure that m ay dam age not only the brain tissue at the bleeding website but in addition in m ore rem ote brain areas. Three t ypes of intracranial hem orrhage may be distinguished based mostly on their relationship to the dura m ater: a Epidural hematoma (epidural = above the dura). The bleeding m ost com m solely happens from a ruptured m iddle m eningeal artery (due to the shut proxim it y of the m iddle m eningeal artery to the calvaria, a sharp bone fragm ent m ay lacerate the artery). The hem atom a form s wager ween the calvaria and the periosteal layer of the dura m ater. Pressure from the hem atom a separates the dura from the calvaria and displaces the brain. The interval guess ween the rst and second loss of consciousness known as the lucid interval (occurs in approxim ately 30�40% of all epidural hem atom as). The bleeding happens into a possible "subdural house," which exist s solely when extravasated blood has dissected the arachnoid m em brane from the dura (the areas are described in C, p. Because the bleeding source is venous, the increased intracranial stress and m ass e ect develop m ore slowly than with an arterial epidural hem orrhage. It is t ypically brought on by a short, sudden rise in blood pressure, like that produced by a sudden rise of intra-abdom inal stress (straining at stool or urine, lifting a heavy object, and so forth. The cardinal symptom of a subarachnoid hem orrhage is a sudden, excruciating headache accom panied by a sti neck attributable to m eningeal irritation. Calvaria Ruptured m iddle m eningeal artery Fracture Arachnoid Dura mater Epidural hematoma a Bridging vein Dura mater Superior sagit tal sinus Falx cerebri Inferior sagit tal sinus Subdural hematoma Subarachnoid area b Subarachnoid house Ruptured aneurysm of an artery at the base of the brain Sphenoid sinus Dura mater c 380 Neuroa natomy 17. Blood Vessels of the Bra in Anterior com m unicating artery Internal carotid artery Posterior com m unicating artery Middle cerebral artery B Sites of berry aneurysms on the base of the brain (after B�hr and Frotscher) the rupture of congenital or acquired arterial aneurysm s at the base of the mind is the m ost frequent reason for subarachnoid hem orrhage and account s for approxim ately 5% of all strokes. These are abnorm al saccular dilations of the circle of Willis and are especially com m on at the website of branching. When certainly one of these thin-walled aneurysm s ruptures, arterial blood escapes into the subarachnoid space. The m ost com m on website is the junction guess ween the anterior cerebral and anterior com m unicating arteries (1); the second m ost probably web site is the branching of the posterior com m unicating artery from the interior carotid artery (2). Corpus callosum Thalamus Caudate nucleus Internal capsule Putam en Hypertensive hem orrhage within the area of the basal ganglia Claustrum Lenticulostriate arteries Globus pallidus Middle cerebral artery C Intracerebral hemorrhag e Coronal part on the degree of the thalam us. Unlike the intracranial extracerebral hem orrhages described above, intracerebral hem orrhage happens when dam aged arteries bleed directly into the substance of the brain. The m ost frequent cause of intracerebral hem orrhage (hem orrhagic stroke) is high blood pressure. The m ost com m on sources of intracerebral bleeding are speci c branches of the m iddle cerebral artery- the lenticulostriate arteries pictured right here (known also because the "stroke arteries"). The hem orrhage causes a dam age to the area of the inner capsule, one e ect of which is to disrupt the pyram idal tract, which passes by way of the capsule (see E, p. The lack of pyram idal tract perform under the lesion is m anifested clinically by spastic paralysis of the lim bs on the alternative facet to the injury (as the pyram idal tract s cross below the extent of the lesion).
500 mg biaxin sale
As a result gastritis symptoms livestrong cheap 250 mg biaxin fast delivery, peripheral m otor facial paralysis is accompanied by listening to loss (deafness) and vestibular dysfunction (dizziness) severe erosive gastritis diet 250 mg biaxin purchase with amex. Hyperacusis due to paralysis of the stapedius m uscle has lit tle medical significance. Classi cation the of Neurovascular Structures Trigem inal ganglion Trigem inal nerve Deep petrosal nerve Internal carotid artery with inside carotid plexus Geniculate ganglion Superior salivatory nucleus Facial nerve Greater petrosal nerve Nucleus of the solitary tract Pterygoid canal with nerve of pterygoid canal St ylom astoid foram en Lingual nerve Chorda t ym pani Subm andibular ganglion Glandular branches Subm andibular gland Lacrim al nerve Maxillary division Lacrim al gland Ophthalm ic division Com m unicating department with zygom atic nerve Zygom atic nerve Sympathetic fibers Mandibular division Pterygopalatine ganglion Nasal glands Sublingual gland C Parasympathetic visceral e erents and visceral a erents (g ustatory bers) of the facial nerve the presynaptic, parasympathetic, visceral e erent neurons are located within the superior salivatory nucleus. Their axons enter and depart the pons with the visceral e erent axons as the nervus interm edius, then journey with the visceral e erent bers arising from the facial m otor nucleus. These preganglionic parasympathetic axons exit the brainstem in the facial nerve and department from it within the larger petrosal nerve, then m ingle with postganglionic sympathetic axons (from the superior cervical ganglion, by way of the deep petrosal nerve) within the nerve of the pterygoid canal. This nerve enters the pteryg opalatine ganglion, where the preganglionic parasym pathetic m otor axons synapse; the sympathetic axons pass through uninterrupted to innervate local blood vessels. The pterygopalatine ganglion provides the lacrim al gland, nasal glands, and nasal, palatine, and pharyngeal m ucosa. Fibers from this ganglion enter the m axillary division and travel (via the com m unicating department of the zygom atic n. Visceral a erent axons (gustatory bers) for the anterior t wo-thirds of the tongue run in the chorda t ympani bers throughout the lingual nerve. The gustatory bers originate from pseudounipolar sensory neurons within the geniculate ganglion, which corresponds to a spinal sensory (dorsal root) ganglion. The chorda t ympani additionally conveys the presynaptic parasympathetic visceral efferent bers for the subm andibular gland, sublingual gland, and sm all salivary glands in the anterior t wo-thirds of the tongue. Most of the axons from the vestibular ganglion time period inate in these 4 nuclei, but a sm aller num ber pass immediately via the inferior cerebellar peduncle into the cerebellum (see Ea). The vestibular nuclei appear as em inences on the oor of the rhom boid fossa (see Eb, p. Two nuclear complexes are distinguished: � Anterior cochlear nucleus � Posterior cochlear nucleus Both nuclei are located lateral to the vestibular nuclei (see Aa, p. They move from the inner ear via the internal acoustic m eatus to the cerebellopontine angle, the place they enter the mind. Nuclei and distribution, ganglia: � V estibular root: the vestibular ganglion accommodates bipolar ganglion cells whose central processes pass to the four vestibular nuclei on the oor of the rhom boid fossa of the medulla oblongata. Their peripheral processes start on the sensory cells of the semicircular canals, saccule, and utricle. Cerebellopontine angle Acoustic neurom a (vestibular schwannom a) Every thorough physical examination should embody a rapid assessment of both nerve components (hearing and stability tests). A lesion of the vestibular root leads to dizziness, while a lesion of the cochlear root results in listening to loss (ranging to deafness). As they grow, they compress and displace the adjoining structures and trigger slowly progressive listening to loss and gait ataxia. Classi cation the of Neurovascular Structures Vestibular ganglion, superior half Anterior ampullary nerve Lateral ampullary nerve Utricular nerve Vestibular root Cochlear root Vestibular ganglion, inferior part Saccular nerve Spiral ganglia Posterior ampullary nerve D Vestibular ganglion and cochlear ganglion (spiral ganglia) the vestibular root and cochlear root nonetheless exist as separate buildings within the petrous a half of the temporal bone. Their axons travel as the vestibular root to the 4 vestibular nuclei on the oor of the rhom boid fossa (further connections are shown on p. An acute lesion of the vestibular organ is m anifested clinically by dizziness (vertigo). It accommodates bipolar sensory cells whose peripheral processes pass to the hair cells of the organ of Corti. Their central processes unite on the oor of the internal auditory canal to type the cochlear root and are distributed to the t wo nuclei which are posterior to the vestibular nuclei. Sites of emergence: the glossopharyngeal nerve emerges from the medulla oblongata and leaves the cranial cavit y via the jugular foram en. Nuclei and distribution, ganglia: � Special visceral e erent (branchiogenic): the nucleus ambiguus sends its axons to the constrictor muscle tissue of the pharynx (= pharyngeal branches, join with the vagus nerve to type the pharyngeal plexus) and to the st ylopharyngeus (see C); � General visceral e erent (parasympathetic): the inferior salivatory nucleus sends parasympathetic presynaptic bers to the otic ganglion. Postsynaptic axons from the otic ganglion are distributed to the parotid gland and to the buccal and labial glands (see a and E); � Somatic a erent: Central processes of pseudounipolar sensory ganglion cells located in the intracranial superior ganglion or extracranial inferior ganglion of the glossopharyngeal nerve term inate within the spinal nucleus of the trigeminal nerve. The peripheral processes of these cells come up from � the posterior third of the tongue, soft palate, pharyngeal mucosa, and tonsils (a erent bers for the gag re ex), see b and c � the m ucosa of the t ympanic cavit y and eustachian tube (t ympanic plexus), see d � the skin of the external ear and auditory canal (blends with the territory supplied by the vagus nerve) and the internal floor of the t ympanic mem brane (part of the t ympanic plexus). Their peripheral processes originate within the posterior third of the tongue (gustatory bers, see e). Developmentally, the glossopharyngeal nerve is the nerve of the third branchial arch. Classi cation the of Neurovascular Structures Lingual branches Tympanic nerve Superior ganglion Inferior ganglion Glossopharyngeal nerve Vagus nerve Branch to st ylopharyngeus m uscle Glossopharyngeal nerve, department to carotid sinus Glossopharyngeal nerve, pharyngeal branches Vagus nerve, branch to carotid sinus Tonsillar branches Pharyngeal plexus Vagus nerve, pharyngeal branches Carotid physique Carotid sinus C Branches of the glossopharyng eal nerve beyond the cranium base Left lateral view. Tympanic nerve Tubarian branch Lesser petrosal nerve Caroticot ympanic nerve Trigem inal nerve Glossopharyngeal nerve Mandibular division Tympanic plexus Auriculotem poral nerve Lesser petrosal nerve Otic ganglion Parotid gland Carotid plexus Tympanic canaliculus with t ympanic nerve Superior ganglion Glossopharyngeal nerve Inferior ganglion Tym panic plexus Postganglionic parasympathetic fibers (run a brief distance with the auriculotemporal nerve) D Branches of the glossopharyngeal nerve within the tympanic cavity Left petrous portion of the temporal bone, frontal view. The t ympanic nerve, which passes by way of the t ympanic canaliculus into the t ympanic cavit y, is the rst branch of the glossopharyngeal nerve. It incorporates visceral e erent (presynaptic parasympathetic) bers for the otic ganglion and som atic a erent bers for the t ympanic cavit y and pharyngot ympanic (eustachian) tube. It joins with sympathetic bers from the carotid plexus (via the caroticot ympanic nerve) to kind the t ympanic plexus. The parasympathetic bers journey as the lesser petrosal nerve to the otic ganglion (see p. E Visceral e erent (parasympathetic) bers of the g lossopharyng eal nerve the presynaptic parasympathetic bers from the inferior salivatory nucleus leave the medulla oblongata with the glossopharyngeal nerve and department o as the t ympanic nerve immediately after emerging from the base of the cranium. The t ympanic plexus provides rise to the lesser petrosal nerve, which leaves the petrous bone by way of the hiatus of the canal for the lesser petrosal nerve and enters the center cranial fossa. Located beneath the dura, it passes by way of the sphenopetrosal ssure to the otic ganglion. Its bers enter the auriculotemporal nerve, move to the facial nerve, and its autonomic bers are distributed to the parotid gland via facial nerve branches. It has the m ost extensive distribution of all the cranial nerves (vagus = "vagabond") and consists of cranial, cervical, thoracic, and stomach parts. This unit deals m ainly with the vagus nerve in the head and neck (its thoracic and belly components are described within the volume on the Internal Organs). Site of emergence: the vagus nerve em erges from the m edulla oblongata and leaves the cranial cavit y by way of the jugular foramen. Nuclei and distribution, ganglia: � Special visceral e erent (branchiogenic): E erent bers from the nucleus ambiguus provide the next m uscles: � Pharyngeal muscles (pharyngeal branch, joins with glossopharyngeal nerve to kind the pharyngeal plexus) and m uscles of the taste bud (levator veli palatini, muscle of the uvula). The peripheral bers originate from � the dura in the posterior cranial fossa (meningeal department, see Df), � the external auditory canal (auricular branch, see Db). Their central processes terminate within the inferior part of the nucleus of the solitary tract. Their peripheral processes provide the next areas: � Mucosa of the lower pharynx at its junction with the esophagus (see Da) � Laryngeal m ucosa above (superior laryngeal nerve) and under (inferior laryngeal nerve) the glot tic aperture (see Da) � Pressure receptors within the aortic arch (see De) � Chem oreceptors within the para-aortic physique (see De) � Thoracic and abdom inal viscera (see Dg) Developmentally, the vagus nerve is the nerve of the fourth and sixth branchial arches. A structure of m ajor clinical importance is the recurrent laryngeal nerve, which supplies viscerom otor innervation to the one m uscle that abduct s the vocal cords, the posterior cricoarytenoid.
Syndromes
- Shock
- Avoid putting your hands in water unless necessary
- Abdominal pain
- Bronchoscopy -- camera down the throat to see burns in the airways and lungs
- Subnormal -- 5 ng/mL
- Malnutrition and dehydration
- Diabetes
- High urine output
Biaxin 500 mg cheap on-line
Arthroscopic double-row suture anchor fixation of minimally displaced greater tuberosity fractures gastritis symptoms in spanish buy cheap biaxin 500 mg online. Arthroscopic discount and fixation with suture-bridge technique for displaced or comminuted larger tuberosity fractures gastritis diet ������� biaxin 500 mg order. Arthroscopic fixation for displaced greater tuberosity fracture using the suture-bridge technique. Arthroscopic fixation technique for comminuted, displaced higher tuberosity fracture. Advantages of arthroscopic transosseous suture restore of the rotator cuff without the utilization of anchors. Dynamic, coordinated contraction of surrounding musculature is necessary to adequately position the glenoid in third-dimensional area, which maximizes the area of contact between the glenoid and the humeral head. More particularly, glenoid positioning is determined by the place of the scapular physique, which is controlled by the synchronous motion of the periscapular musculature. When glenohumeral motion is initiated, the scapula must tilt, rotate, protract, and/or retract to compensate for the position of the humeral head. To obtain these motions, the concave scapular body must glide smoothly over the convex posterior thorax with assistance from strategically positioned muscular tissue and interposed bursae. Therefore, anatomic derangements within the scapulothoracic area can produce disordered glenohumeral kinematics, resulting in painful bursitis with or with out mechanical crepitus. These situations are sometimes collectively referred to as snapping scapula syndrome and/or scapulothoracic bursitis. The big selection of attainable signs related to these situations may be categorized based on the most likely etiology. For example, scapulothoracic incongruence on account of space-occupying skeletal or soft-tissue lesions, kyphoscoliotic posture,1 or predisposing anatomic variation, similar to hyperangulation of the superomedial scapular angle or the presence of a socalled Luschka tubercle, 2-4 are more doubtless to generate symptoms associated to mechanical crepitation. In distinction, sufferers who complain of ache in the absence of mechanical symptoms are extra doubtless to have symptomatic bursitis, typically because of continual overuse. However, though this basic classification may be useful, it is necessary to recognize that symptomatic bursitis can result in mechanical crepitation (via bursal fibrosis5-8), while mechanical crepitation can lead to symptomatic bursitis (via disordered scapular motion). This axial magnetic resonance imaging slice demonstrates a outstanding superomedial angle (yellow arrow) in a affected person with recalcitrant scapulothoracic bursitis and mechanical crepitus. Arthroscopic excision of pathologic bursal tissue and bony resection of the superomedial scapular angle have each been discovered to present important improvements in pain and performance in the majority of patients. Indications Symptoms persist regardless of three to 6 months of applicable nonoperative therapy. Mechanical crepitus is persistent throughout intraoperative dynamic examination regardless of removing of pathologic bursal tissue. The operative extremity and posterior thorax are extensively ready and draped using a sterile method. This so-called rooster wing position induces a physiologic posterior scapular tilt, which enlarges the operative subject and aids in arthroscopic visualization. In addition, medial portal positioning mitigates the chance for intrathoracic penetration, which can occur when arthroscopic instruments are inserted into the scapulothoracic space at an acute angle. This preoperative photograph demonstrates the "chicken wing" position by which the dorsum of the forearm is placed over the lumbar backbone. This position subjects the humerus to nearly maximal inside rotation, which forces the scapula to tilt posteriorly, thus increasing the out there operating space between the anterior scapula and the posterior chest wall. When further house is needed for visualization through the procedure, application of a medially directed pressure on the proximal humerus could assist enhance the volume of the scapulothoracic space via "bayonet apposition. Illustration depicting the necessary neurovascular anatomy related to scapulothoracic bursectomy and superomedial angle resection. Arthroscopic portals ought to be established no less than 3 cm medial to the medial scapular border to keep away from iatrogenic harm to the dorsal scapular nerve and artery, which run collectively beneath the rhomboid major, rhomboid minor, and levator scapulae muscle tissue. In addition, danger of injury to the spinal accent nerve may be minimized by establishing portals inferior to the extent of the scapular backbone. The suprascapular nerve and artery are hardly ever in danger until an accessory superior portal is needed to complete the procedure or extreme lateral dissection is undertaken. Prior to the insertion of arthroscopic devices, approximately 100 mL of saline combined with native anesthetic and epinephrine is injected deep to the superomedial angle to both broaden the infraserratus bursa for adequate visualization and to present hemostasis through the process. The image inset is an arthroscopic view of the spinal needle placed on the superomedial angle. Step-by-Step Description of the Procedure A small stab incision is made roughly 3 cm medial to the inferomedial angle and a 30-degree arthroscope is inserted, taking care to remain as parallel to the chest wall as potential. Care ought to be taken to maintain a fluid pump strain of less than 50 mm Hg throughout the process to avoid excessive fluid extravasation into surrounding tissues. A spinal needle is inserted roughly 3 cm medial to the medial scapular border at some extent just inferior to the extent of the scapular spine, marking the placement of the medial working portal. Once this portal is established, diagnostic arthroscopy is performed utilizing each the 30- and 70-degree arthroscopes to accurately localize the superomedial scapular angle. Using the previously positioned spinal needle for orientation, debridement is sustained till the superomedial scapular angle is completely exposed. When necessary, access to the supraserratus bursa could be achieved by bluntly penetrating the laterally positioned serratus anterior muscle. If mechanical crepitus remains to be present and skeletal impingement remains to be visible following complete bursectomy, superomedial angle resection is then carried out. Note that a triangular part of the superomedial scapular angle has previously been resected (arrow). Although a triangular part of bone is often removed approximately 2 cm superoinferiorly and three cm mediolaterally, you will want to mark the extent of the deliberate resection in every case utilizing a quantity of spinal needles, relying on the diploma and location of scapulothoracic impingement. This method facilitates complete, correct bony resection of the superomedial angle without rising the risk to close by vascular structures. The operative extremity is again positioned by way of a variety of motion whereas immediately visualizing the scapulothoracic space by way of both portals to confirm each sufficient resection and the presence of a easy articulating floor. The portal sites are closed using a regular method, a simple sling is utilized, and the patient is transferred to the post-anesthesia care unit. Arthroscopic Bursectomy and Superomedial Angle Resection 283 Postoperative Protocol Active and passive vary of movement exercises, such as scapular protraction, retraction, and rotation, are begun immediately postoperatively with a development towards glenohumeral strengthening at roughly 4 weeks adopted by periscapular strengthening at roughly 8 weeks. Most patients return to sports after 3 months of structured and supervised rehabilitation. In all circumstances, bodily therapy protocols should be individualized according to affected person tolerance and progress. Potential Complications Although uncommon, there are a quantity of important surgical complications distinctive to this procedure that can be prevented through the use of acceptable arthroscopic methods. Injury to the dorsal scapular artery and/or nerve can occur when arthroscopic portals are positioned < 3 cm medial to the medial scapular border. The spinal accessory nerve can additionally be at risk when an arthroscopic portal is placed superior to the level of the scapular backbone. Placing the operative limb in the "chicken wing" position will increase the potential house between the scapula and the posterior chest wall, which improves arthroscopic visualization.
Generic 250 mg biaxin otc
Remplissage repair � new frontiers within the prevention of recurrent shoulder instability: a 2-year follow-up comparative research chronic gastritis mayo 500 mg biaxin generic free shipping. The evaluation of arthroscopic remplissage by high-resolution magnetic resonance imaging gastritis symptoms home treatment 500 mg biaxin free shipping. Hill-Sachs remplissage, an arthroscopic resolution for partaking Hill-Sachs lesion: 2- to 10-year follow-up and incidence of recurrence. Arthroscopic Bankart repair and remplissage in patients with combined humeral and glenoid bone loss. The effect of the remplissage process on shoulder stability and range of motion. The impact of the remplissage process on shoulder range of movement: a cadaveric study. These historic open procedures have progressed to arthroscopic options that have shown wonderful outcomes. Arthroscopic strategies have advanced from arthroscopic inferior capsular shift using a transglenoid technique3-5 initially reported on by Duncan and Savoie5 in 1993, to arthroscopic stabilization with bioabsorbable tacks. The arthroscopic, all-inside approach was described by Wichman and Synder in 1997. The imbalance that results can result in impingement, periscapular dyskinesis, and rotator cuff pathology, all of which may be ache turbines. Open inferior capsular shift has been used successfully in patients whom have failed nonoperative administration. Combining a radical history with patient remark can often give a considerable quantity of information. Typically, the chief complaint is pain, normally associated with motion, whether from an overhead sport or making an attempt to raise heavy objects. Check for proof of hyperextensibility or changes within the pores and skin texture, corresponding to velvety or unfastened skin, that might recommend hyperlaxity. These various presentations underscore the necessity for the physician to outline the underlying pathology and distinguish instability from laxity. History of multiple previous subluxating episodes or dislocation occasions caused by a traumatic or volitional occasion Repetitive microtrauma to the labrum because of recurrent subluxation causes lack of chondrolabral restraint and additional instability. These adjustments can lead to capsular stretching, which may present as symptomatic laxity. In addition to testing for multidirectional instability, one ought to evaluate for anterior and posterior instability as well as carry out a radical neurovascular exam. A sulcus sign is broadly thought of the gold standard test for evaluating multidirectional instability, although it has been shown to have a excessive specificity and a low sensitivity. A constructive test will show dimpling, > 2 cm displacement from the acromion, and a palpable "sulcus" underneath the acromion as the arm is pulled inferiorly. The load and shift test is carried out with the patient supine on the examination desk whereas the doctor facilities the humeral head by applying an axial drive then translates the head. The examination is graded based on how much the humeral head shifts in relation to the glenoid. A classification of grade 1 occurs when the humeral head can be translated to the glenoid rim, grade 2 occurs when the humeral head could be dislocated and lowered spontaneously, and grade 3 occurs when the pinnacle may be dislocated however not decreased spontaneously. The Gagey hyperabduction take a look at is most useful for evaluating inferior glenohumeral ligament translation. It has been proven that an asymptomatic patient will typically abduct no more than 90 degrees. If bone loss is a concern, a computed tomography scan could additionally be helpful to assist with surgical planning. The surgical procedure may also be carried out within the beach chair position if most well-liked by the surgeon. The double-loaded suture anchors in place on the most inferior level of attachment. Step-by-Step Description of the Procedure the affected person is examined within the supine position by performing the load and shift check while the affected person is anesthetized to verify the prognosis. The authors suggest examining the contralateral shoulder to get an concept of the baseline to return the injured shoulder to . Patient is then placed in the lateral decubitus place using an axillary roll, guaranteeing all bony prominences are nicely padded and the peroneal nerve is free. Placing the patient in the lateral place will allow wonderful access to the anterior, posterior, and inferior features of the glenohumeral joint, where the majority of the attention shall be during the surgical procedure. After the arm is prepped and draped and then hung with the preferred gadget by the surgeon, roughly 5 to 7 lbs of traction are used to droop the arm. It is essential to not overuse traction as this will trigger neurologic issues. Create the posterior portal, which ought to be barely more lateral than ordinary to enable for higher angulation in the case that a posterior anchor will want to be placed. Complete a radical inspection of the glenohumeral joint, with cautious analysis of the biceps anchor; the interval; and the anterior, inferior, and posterior capsule, documenting the looks and laxity of the ligamentous constructions. Placing the arthroscope in the anterior portal and viewing posteriorly is important for a whole evaluation and for the remedy of posterior pathology. Evaluate the anterior and posterior labrum and glenoid rim to assess bony loss and harm. Begin by repairing any displaced labral pathology through the use of an anchor to create a base to which the capsule may be plicated to . Repair the labrum with double-loaded suture anchors at the most inferior point of attachment. Simple or horizontal mattress suture configuration can be utilized and is helpful to keep the knots away from the glenohumeral joint to avoid symptoms of clicking and catching postoperatively. Portal placement above the subscapularis is important for the right angle of anchor placement. More superiorly, the authors usually use small single-loaded anchors as needed. If the labral advanced appears intact but is of poor high quality (eg, Kim lesion), the authors suggest augmenting the labrum-plication restore using a 1. In this way, the authors each plicate the capsule and restore any splits or weak points within the labrum. Postoperative Protocol Protect the patient in an abduction pillow brace for four to 6 weeks, then instruct the patient to begin performing active vary of motion workouts on his or her personal for 3 weeks. Physical therapy could be started at 8 weeks; presently, formal bodily remedy is begun where the affected person works on lively and active-assisted range of movement. It is typically 6 months before the patient is allowed to take part in contact sports.
Generic biaxin 500 mg without prescription
Nonsurgical management has historically been advocated for all but the most high-level athletes gastritis in cats purchase biaxin 250 mg mastercard. Most sufferers treated nonoperatively can expect a great functional outcome and a return to earlier levels of exercise gastritis diet plan uk purchase biaxin 500 mg line. However, some authors advocate early surgical intervention in high-demand athletes and heavy handbook laborers. Although some patients still have a distal clavicle prominence, most will do properly with nonoperative management. Those sufferers with persistent horizontal instability, diagnosed primarily by crepitation and horizontal (anteroposterior) movement of the clavicle on the acromion with resisted cross chest adduction and abduction, will normally experience a poor outcome and can more than likely desire surgical reconstruction. Supplementation of the restore with an artificial materials or implant to keep stability in the course of the acute phase of healing2 86 Chapter 8 Each construct consists of a stent and a biologic element. The use of the biologic element may differ with the timing of the surgery and the severity of the injury. Arthroscopic-Assisted Anatomic Coracoclavicular Ligament Reconstruction With Looped Allograft Positioning the patient is positioned within the lateral decubitus place, rolled back 30 levels. The neck is directed 10 to 15 levels laterally away from the operative site to enable for better access and to avoid interference with laterally directed drill approaches during the case. The clavicle, acromion, and coracoid are palpated and marked as a guide for portal placement. Portal Placement and Initial Arthroscopic Approach An arthroscope is then launched through a regular posterior portal into the glenohumeral joint for diagnostic arthroscopy. Once diagnostic arthroscopy and concomitant procedures are full, the arthroscope is removed from the glenohumeral joint and placed into the subacromial space by way of the same posterior skin portal. A lateral portal three cm distal to the anterolateral nook of the acromion is then established using an outside-in method with a spinal needle while visualizing from the posterior portal. An anterior portal is made immediately anterior and barely inferior to the medial coracoid by use of an outside-in approach with a spinal needle. Damage to the nearby neurovascular buildings is averted by maintaining the electrocautery in shut contact with bone always. It may be essential to release the pectoralis minor tendon from the medial floor of the coracoid at this time, especially in cases of chronic contracture refractory to preoperative stretching, or in cases the place visualization of the coracoid is unsatisfactory. The undersurface of the clavicle is identified and uncovered with an electrocautery gadget and a shaver to improve visualization. A lateral viewing portal is used to verify outside-in placement of the anterior portal. The superior and inferior surfaces of the coracoid are debrided using electrocautery. The energetic surface is all the time kept involved with the bone of the coracoid to avoid neurologic harm. Dissection with a needle-tip electrocautery is accomplished to the extent of the deltotrapezial fascia. Homan retractors are positioned anterior and posterior to the clavicle to visualize the distal clavicle. The surface of the cautery is kept in contact with the bone of the displaced clavicle. The insertion factors are confirmed arthroscopically, and the wires are over-reamed with a 5-mm reamer. Graft Passage Visualization continues via the anterolateral portal and a passing suture is inserted via the anterior portal, directed underneath the coracoid, and retrieved out of the medial clavicular tunnel. A second passing suture is then placed by way of the anterior cannula, retrieved superior to the coracoid, and pulled out the lateral clavicular tunnel. The medial suture is used to pull the graft from the anterior portal, beneath the coracoid, and thru the medial clavicular tunnel, thus exiting the incision. The passing suture is placed via the anterior portal, retrieved inferior to the coracoid, and pulled out of the medial clavicular tunnel. A second passing suture (purple) is passed via the anterior portal, retrieved superior to the coracoid, and transferred out of the lateral clavicular tunnel. The green passing suture is used to lead the semitendinosus graft inferior to the coracoid and out of the medial clavicular tunnel. Viewing from the lateral portal, the graft is adopted because it moves up and into the medial clavicular tunnel. The second passing suture pulls the alternative end of the graft via the cannula, over the coracoid, and into the lateral clavicular tunnel. The graft is in place and tensioned to get rid of soft tissue constraints or laxity, and satisfactory positioning is confirmed. Note the 2 limbs of the graft cross within the house between the coracoid and clavicle. Anatomic Coracoclavicular Reconstruction With Tendon Graft and Cortical Fixation Button the arthroscope is introduced into the glenohumeral joint utilizing the usual posterior portal. Some authors choose to keep the arthroscope within the joint, excise the rotator interval, and continue to view from this portal through the process. The authors prefer to use the same anterior and lateral portals described previously. The preliminary levels of coracoid exposure are as previously detailed in the graft method. The semitendinosus allograft is looped through the hook plate and across the coracoid. Dissection to the extent of the deltotrapezial fascia is carried out with electrocautery. With the clavicle adequately visualized, the clavicular drill holes are made with the same technique as described beforehand. The fixation button is then passed via the conoid gap within the clavicle and inferiorly through the coracoid, and the button is flipped beneath the coracoid. A passing suture is positioned across the coracoid in a medial-to-lateral trend and posterior to the conjoined tendon. The graft is passed around the coracoid and thru the corresponding clavicle hole. Hook Plate Fixation (Nonarthroscopic Technique) For cases during which extra inflexible fixation is desired, a hook plate may be used because the "stent. Postoperative Protocol Arthroscopic Postoperatively, the shoulder is supported with a shoulder immobilizer and abduction pad full-time for 6 weeks. A dynamic scapular retraction brace is worn starting at four weeks following surgery to be used during daytime actions, and the abduction sling is steadily discontinued. Active vary of motion can be started at that time, but cross chest adduction is averted until 8 weeks postoperatively. At 6 to eight weeks, aggressive rehabilitation is started with a return to normal activities, often by 12 to 16 weeks following restore. One week postoperatively, the sling is discontinued except at evening and bodily therapy is then initiated. After four months, the plate is eliminated and the patient is followed radiographically at monthly intervals to monitor for any erosion into the scapular backbone.
Biaxin 250 mg discount online
Care ought to be taken when using these devices as the sharp needles can cut or nick previously positioned sutures gastritis symptoms causes treatments and more buy 250 mg biaxin. Super-sutures decrease the incidence of suture breakage during knot tying gastritis symptoms nhs direct biaxin 250 mg order line, which minimizes this previously widespread expertise with standard power suture. Super-sutures are rather more proof against fraying than typical suture materials. Super-sutures can be quite slippery, and a few investigators have reported a tendency for knot slippage with out suture breakage with numerous super-sutures. It is useful to benefit from the objective feedback supplied by a knot tester if possible in order to maximize proficiency across the vary of supplies which are prone to be used in the working room. Some super-sutures are so robust that they induce glove tears and finger lacerations during arthroscopic shoulder surgery. More importantly, skin lacerations are a mirrored image of the amount of drive that can be applied by super-sutures throughout the glove and into the finger. Surgeons should be mindful of glove tears during surgery so as to decrease the danger of bacterial contamination from the pores and skin of the surgeon. Specific Arthroscopic Knots (Sliding and Nonsliding) Many arthroscopic knots are well-described in the literature. Most knots work well so long as the surgeon understands and adheres to basic ideas of knot security and loop safety, including correct use of again up halfhitches. Every arthroscopic surgeon must be comfy with no less than 2 "go-to" knots for the 6 Chapter 1 working room. It is efficient and effective to turn into facile and technically consistent with no less than one sliding knot, one nonsliding knot, and, if potential, one sliding-locking knot. Sliding knots are advantageous because the knot is configured outside of the arthroscopic cannula. The knot is then delivered to the target location by the submit strand sliding through tissue and the suture anchor. It is therefore essential to routinely assess suture sliding before creating the knot. Sliding knots require a shortened publish, which returns to acceptable working length because the knot is delivered and the publish is retrieved. Some surgeons choose to use a nonsliding knot routinely, which is composed of a sequence of reversed halfhitches on alternating posts. The main driver of success is meticulous surgical approach and attention to element, versus particular knot choice. There are occasions throughout surgery when a sliding-locking knot is advantageous, such as when the repair tends to "spring back" from the goal tissue. This tendency can create loop growth and related gap formation at the restore web site in the transient second between main knot placement and half-hitch delivery. The approach for delivering and securing a sliding-locking knot involves 3 sequential steps: 1. Tripping and locking the knot by pulling on the non-post limb It is necessary to remove all loop slack by deliberate pretension of the post limb. Surgical assistants, notably the individual holding the arthroscope, ought to watch the monitor carefully throughout this stage of the process. It is essential to advise the operating surgeon if the loop loosens at any point during knot tying as a end result of this is a correctable downside whether it is recognized earlier than the position of additional half-hitches. Arthroscopic knot security is achieved by the position of no less than three reversed throws on alternating posts to back up the preliminary knot. Riboh et al16 demonstrated that shortcut methods (tensioning of half-hitches with out switching of the knot pusher) can outcome in decreased knot performance after the location of a base Tennessee slider. In some circumstances, the gentle tissues being repaired are of poor high quality (eg, a previously operated and degenerative rotator cuff tendon). In this situation, strong anchors, robust sutures, and good knots can fail if the suture rips through tissue itself. Gerber and colleagues18 famous that final tensile energy was significantly increased by the modified Mason-Allen suture with Arthroscopic Knot Tying 7 open rotator cuff approach. This greedy suture includes three passes of suture via tendon, which provides a self-locking mechanism when rigidity is applied. This was most likely caused by slight slack in the complicated suture loops, which created a gap during low-level cyclic load. Therefore, you will need to gently remove slack from sutures, especially from advanced grasping sutures, prior to "setting" of the arthroscopic knot. The large cuff sew is created by placing an preliminary simple loop transverse to the fibers of the rotator cuff. This loop is tied initially, then a simple suture from an anchor is handed medial to the initial suture loop. When the straightforward suture is tied, pressure is partially born by the initial transverse suture loop, which decreases the tendency for tissue cut out. This configuration was noted to be roughly 4 occasions stronger than a simple suture or horizontal mattress suture and roughly equal to the load to failure of an openly placed modified Mason-Allen sew. The mattress is tied first, and when the straightforward suture is introduced beneath pressure, it engages the mattress limbs. Practice Boards and Knot Tester Recent research suggest that knot-tying efficiency and consistency may be lower than desired, even in the hands of skilled surgeons. Historically, most training has sometimes concerned follow on knot-tying boards, utilizing written instructions and/or video demonstrations which are emulated by the learner. Evaluation of knot-tying expertise is usually limited to subjective observation and evaluation by a extra skilled mentor. Some investigators describe self-evaluation instruments that may increase the effectiveness of knot-tying instruction. Unfortunately, the use of sophisticated material testing units may be cost-prohibitive and impractical for most studying labs. Suture tangling could be avoided by cautious and preplanned management of sutures so as to maintain only the two working strands throughout the working cannula throughout knot tying. Extra sutures within the cannula considerably enhance the danger of entrapment within the knot, which can be troublesome to correct. The incidence of suture breakage has been decreased by supersutures, but rupture can still happen if the surgeon is simply too rough. The likelihood of suture breakage will increase with nicks and fraying, which could be minimized by taking care with sharp suture passing devices and "stabber-graspers. A clear dome with multiple portals facilitates apply via cannulas beneath direct visualization. The first notch on the loop-sizer matches the knot-tying mandrel of the base station.
Biaxin 250 mg without prescription
The outer lipid layer gastritis anxiety cheap biaxin 250 mg free shipping, produced by the Meibom ian glands hcg diet gastritis buy cheap biaxin 500 mg on-line, defend s the aqueous m iddle layer of the tear lm from evaporating. E Obstructions to lacrimal drainag e (after Lang) Sites of obstruction within the lacrim al drainage system can be located by irrigating the system with a special uid. To m ake this determ ination, the exam iner m ust be fam iliar with the anatomy of the lacrim al apparatus and the norm al drainage pathways for lacrim al uid (see A). In b the uid re uxes via the inferior lacrim al canaliculus, and in c it ows via the superior lacrim al canaliculus. When the entire lacrim al sac has lled with uid, the uid begins to re ux into the superior lacrim al canaliculus. Most of the eyeball is composed of three concentric layers (from outside to inside): the sclera, choroid, and retina. The outer coat of the eye in this region is kind ed by the cornea (anterior portion of the brous coat). As the "window of the eye," it bulges ahead while overlaying the structures behind it. At the corneoscleral lim bus, the cornea is continuous with the much less convex sclera, which is the posterior portion of the outer coat of the eyeball. It is a rm layer of connective tissue that offers at tachm ent to the tendons of all the extraocular m uscles. Anteriorly, the sclera within the angle of the anterior cham ber form s the trabecular m eshwork (see p. On the posterior facet of the eyeball, the axons of the optic nerve pierce the lam ina cribrosa of the sclera. It consist s of three part s within the anterior portion of the attention: the iris, ciliary body, and choroid, the lat ter being distributed over the entire eyeball. Its root is steady with the ciliary physique, which accommodates the ciliary m uscle for visual accom m odation (alters the refractive energy of the lens, see p. The ciliary physique is continuous on the ora serrata with the m iddle layer of the eye, the choroid. The choroid organ is the m ost extremely vascularized region within the physique and serves to regulate the tem perature of the attention and to supply blood to the outer layers of the retina. The internal layer of the attention is the retina, which includes an internal layer of photosensitive cells (the sensory retina) and an outer layer of retinal pigm ent epithelium. The lat ter is continued forward as the pigm ent epithelium of the ciliary body and the epithelium of the iris. Incident gentle is norm ally centered onto the fovea centralis, which is the site of greatest visible acuit y. The inside of the eyeball is occupied by the vitreous humor (vitreous body, see C). Orga ns and Their Neurovascula r Structures Cornea Site of at tachm ent to ora serrata (vitreous base of Salzm ann) Site of at tachm ent to posterior lens capsule (Wieger ligam ent) Hannover area Garnier space Meridian Petit space Berger space Hyaloid canal At tachm ent to optic disk (Martegiani ring) Optic nerve Vitreous body Optic nerve Equator B Reference traces and points on the eye the line m arking the greatest circum ference of the eyeball is the equator. Myopia (nearsightedness) Incident gentle rays Norm al (em m etropic) eye Hyperopia (farsightedness) C Vitreous physique (vitreous humor) (after Lang) Right eye, transverse section considered from above. Sites the place the vitreous physique is at tached to other ocular buildings are proven in red, and adjoining areas are shown in green. The vitreous body stabilizes the eyeball and defend s towards retinal detachm ent. Devoid of nerves and vessels, it consist s of 98% water and 2% hyaluronic acid and collagen. For the treatm ent of som e diseases, the vitreous physique m ay be surgically rem oved (vitrectomy) and the resulting cavit y lled with physiological saline resolution. Eyeball Superior oblique Cornea Lens Retina Superior rectus Medial rectus Lateral rectus D Light refraction in a normal (emmetropic) eye and in myopia and hyperopia Parallel rays from a distant mild source are norm ally refracted by the cornea and lens to a focal point on the retinal floor. Because of this disparit y, the purpose of m axim um visible acuit y, the fovea centralis, is lateral to the "blind spot" of the optic disk (see A). The lens is at tached by rows of brils (zonular bers) to the ciliary m uscle, whose contractions alter the form and focal length of the lens (the structure of the ciliary physique is shown in B). The lens is a dynam ic construction that can change it s shape in response to visible requirem ent s (see Cb). The anterior cham ber of the attention is situated in front of the lens, and the posterior cham ber is located wager ween the iris and the anterior epithelium of the lens (see p. The lens, like the vitreous body, is devoid of nerves and blood vessels and is com posed of elongated epithelial cells - the lens bers. Anterior cham ber Posterior cham ber Scleral spur Cornea Iris Canal of Schlem m Ocular conjunctiva Ciliary m uscle Sclera Pars plana Pars plicata Lens Zonular fibers Epithelium of ciliary body Trabecular m eshwork Ciliary physique Lens Iris Ciliary physique, pars plicata Ciliary physique, pars plana B the lens and ciliary physique Posterior view. The curvature of the lens is regulated by the m uscle bers of the annular ciliary body (see Cb). The lat ter part is ridged by approxim ately 70�80 radially-oriented ciliary processes, which encompass the lens like a halo when considered from behind. The ciliary processes include giant capillaries, and their epithelium secretes the aqueous hum or (see p. Very ne zonular bers extend from the basal layer of the ciliary processes to the equator of the lens. These bers and the spaces bet ween them constitute the suspensory apparatus of the lens, known as the zonule. Most of the ciliary body is occupied Sclera Choroid Zonular fibers Ciliary processes Ciliary m uscle Ora serrata Retina, optical half by the ciliary m uscle, a sm ooth m uscle com posed of m eridional, radial, and circular bers. It arises m ainly from the scleral spur (a reinforcing ring of sclera slightly below the canal of Schlem m), and it at taches to buildings together with the Bruch m em brane of the choroid and the inside surface of the sclera. When the cili- ary m uscle contracts, it pulls the choroid ahead and relaxes the zonular bers. Orga ns and Their Neurovascula r Structures Ciliary m uscle relaxed, zonular fibers tense, lens flat tened Equator Lens capsule Light rays in distant accom m odation Lens Anterior pole Posterior pole Light rays in close to accom m odation a Axis b Ciliary m uscle contracted, zonular fibers lax, lens m ore rounded C Reference traces and dynamics of the lens a Principal reference lines of the lens: the lens has an anterior and posterior pole, an axis passing wager ween the poles, and an equator. The lens has a biconvex shape with a larger radius of curvature posteriorly (16 m m) than anteriorly (10 m m). It s operate is to transm it light rays and m ake ne adjustm ent s in refraction. It s refractive power ranges from 10 to 20 diopters, depending on the state of accom m odation. Due to the constant proliferation of epithelial cells, that are all rm ly incorporated within the lens capsule, the tissue of the lens becom es more and more dense with age. A slit-lamp examination ination will dem onstrate zones of various cell densit y (zones of discontinuit y). The zone of highest cell densit y, the embryonic nucleus, is at the center of the lens. The childish nucleus develops after birth, and nally the grownup nucleus begins to form in the course of the third decade of life. Descem et m em brane Endothelium E Structure of the cornea the cornea is roofed externally by nonkeratinized strati ed squam ous epithelium whose basal m em brane borders on the anterior lim iting lam ina (Bowm an m em brane).

