Allopurinol
Allopurinol dosages: 300 mg
Allopurinol packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills

Buy 300 mg allopurinol otc
Cahen D gastritis symptoms pdf cheap allopurinol 300 mg, et al: Longterm results of endoscopic drainage of frequent bile duct strictures in chronic pancreatitis no xplode gastritis 300 mg allopurinol with visa, Eur J Gastroenterol Hepatol 52:55�63, 2005. Choudhary A, et al: Effect of precut sphincterotomy on postendoscopic retrograde cholangiopancreatography pancreatitis: a systematic evaluation and metaanalysis, World J Gastroenterol 20(14):4093�4101, 2014. Costamagna G, Boskoski I: Current treatment of benign biliary stric tures, Ann Gastroenterol 26(1):37�40, 2013. Costamagna G, et al: Longterm results of endoscopic administration of postoperative bile duct strictures with rising numbers of stents, Gastrointest Endosc 54(2):162�168, 2001. Domagk D, et al: Endoscopic retrograde cholangiopancreatography in bile duct strictures: a prospective comparability of imaging diagnostics with histopathological correlation, Am J Gastroenterol 99(9):1684� 1689, 2004. Donelli G, et al: Plastic biliary stent occlusion: factors involved and attainable preventive approaches, Clin Med Res 5:53�60, 2007. Draganov P, et al: Longterm outcome in patients with benign biliary strictures treated endoscopically with a number of stents, Gastrointest Endosc 55(6):680�686, 2002. Elek G, et al: Histological evaluation of preoperative biopsies from ampulla vateri, Pathol Oncol Res 9:32�41, 2003. Fumex F, et al: Similar performance but higher cholecystitis price with coated biliary stents: results from a prospective multicenter evalu ation, Endoscopy 38(8):787�792, 2006. Gabbert C, et al: Advanced methods for endoscopic biliary imaging: cholangioscopy, endoscopic ultrasonography, confocal, and beyond, Gastrointest Endosc Clin N Am 23(3):625�646, 2013. Garrow D, et al: Endoscopic ultrasound: a metaanalysis of take a look at per formance in suspected biliary obstruction, Clin Gastroenterol Hepatol 5(5):616�623, 2007. Gupta K, et al: Endoscopic ultrasoundassisted bile duct entry and drainage: multicenter, longterm analysis of strategy, outcomes, and complications of a technique in evolution, J Clin Gastroenterol 48(1):80�87, 2014. Herreros de Tejada A, et al: Doubleguidewire method for difficult bile duct cannulation: a multicenter randomized, managed trial, Gastrointest Endosc 70(4):700�709, 2009. Irani S, et al: Papillectomy for ampullary neoplasm: outcomes of a single referral heart over a 10year interval, Gastrointest Endosc 70:923�932, 2009. A potential randomized controlled trial, J Gastroenterol 45(11):1183�1191, 2010. Itoi T, et al: Endoscopic ultrasonographyguided cholecystogastros tomy utilizing a lumenapposing metallic stent as an different selection to further hepatic bile duct drainage in pancreatic cancer with duodenal invasion, Dig Endosc 25(Suppl 2):137�141, 2013. Iwano H, et al: Unilateral versus bilateral drainage using selfexpandable metallic stent for unresectable hilar biliary obstruction, Dig Endosc 23:43�48, 2011. Iwashita T, et al: Endoscopic ultrasoundguided biliary drainage: a review, Clin J Gastroenterol 7:94�102, 2014. Jakobs R, et al: Fluoroscopically guided laser lithotripsy versus further corporeal shock wave lithotripsy for retained bile duct stones: a potential randomized examine, Gut 40:678�682, 1997. Kaassis M, et al: Plastic or steel stents for malignant stricture of the widespread bile duct Kaffes A, et al: Metal stent versus plastic stent for submit liver transplant anastomotic biliary strictures [abstract], Endoscopy 44(Suppl):A97, 2012. Kahaleh M, et al: Temporary placement of coated selfexpandable metallic stents in patients with biliary leak: midterm evaluation of a pilot study, Gastrointest Endosc 66:52�59, 2007. Kahaleh M, et al: Unresectable cholangiocarcinoma: comparability of survival in biliary stenting alone versus stenting with photodynamic remedy, Clin Gastroenterol Hepatol 6(3):290�297, 2008. Kalaitzakis E, et al: Diagnostic and therapeutic utility of single operator peroral cholangioscopy for indeterminate biliary lesions and bile duct stones, Eur J Gastroenterol Hepatol 24(6):656�664, 2012. Kapetanos D, et al: Case series of transpancreatic septotomy as precut ting approach for difficult bile duct cannulation, Endoscopy 39(9): 802�806, 2007. Kato H, et al: Short doubleballoon enteroscopy is feasible and effective for endoscopic retrograde cholangiopancreatography in patients with surgically altered gastrointestinal anatomy, Dig Endosc 26 (Suppl 2):130�135, 2014. Kedia P, et al: Endoscopicguided biliary drainage: how can we obtain environment friendly biliary drainage Kitajima Y, et al: Usefulness of transpapillary bile duct brushing cytol ogy and forceps biopsy for improved analysis in patients with biliary strictures, J Gastroenterol Hepatol 22:1615�1620, 2007. Larghi A, et al: Management of hilar biliary strictures, Am J Gastroenterol 103(2):458�473, 2008. Manes G, et al: An evaluation of the factors related to the develop ment of complications in patients undergoing precut sphincterot omy: a potential, controlled, randomized, multicenter research, Am J Gastroenterol 104(10):2412�2417, 2009. Manta R, et al: Linear endoscopic ultrasonography vs magnetic reso nance imaging in ampullary tumors, World J Gastroenterol 16:5592� 5597, 2010. MalufFilho F, et al: Rotatable sphincterotome facilitates bile duct cannulation in patients with altered ampullary anatomy, Gastroenterol Hepatol 4(1):59�62, 2008. Maydeo A, Bhandari S: Balloon sphincteroplasty for removing tough bile duct stones, Endoscopy 39(11):958�961, 2007. Meining A, et al: Direct visualization of indeterminate pancreaticobili ary strictures with probebased confocal laser endomicroscopy: a multicenter experience, Gastrointest Endosc 74:961�968, 2011. Meining A, et al: Classification of probebased confocal laser endomi croscopy findings in pancreaticobiliary strictures, Endoscopy 44(3): 251�257, 2012. Menezes N, et al: Prospective evaluation of a scoring system to predict choledocholithiasis, Br J Surg 87:1176�1181, 2000. Personal expertise and evaluate of the literature, Eur J Ultrasound 10(2�3):105�115, 1999. Mukai I, et al: Metallic stents are more efficacious than plastic stents in unresectable malignant hilar biliary strictures: a randomized con trolled trial, J Hepatobiliary Pancreat Sci 20:214�222, 2013. Naitoh I, et al: Unilateral versus bilateral endoscopic metal stenting for malignant hilar biliary obstruction, J Gastroenterol Hepatol 24:552� 557, 2009. Nakai Y, et al: Confocal laser endomicroscopy in gastrointestinal and pancreatobiliary illnesses, Dig Endosc 26(1):86�94, 2014. Natsui M, et al: Longterm outcomes of endoscopic papillary balloon dilation and endoscopic sphincterotomy for bile duct stones, Dig Endosc 25(3):313�321, 2013. Navaneethan U, et al: Early precut sphincterotomy and the risk of endoscopic retrograde cholangiopancreatography related complica tions: an updated metaanalysis, World J Gastrointest Endosc 6(5):200�208, 2014. Navaneethan U, et al: Precut sphincterotomy: efficacy for ductal access and the danger of opposed events, Gastrointest Endosc 81(4):924�931, 2015. Navaneethan U, et al: Comparative effectiveness of biliary brush cytol ogy and intraductal biopsy for detection of malignant biliary stric tures: a scientific evaluate and metaanalysis, Gastrointest Endosc 81(1):168�176, 2015. Nehaus H, et al: Randomized study of intracorporeal laser lithotripsy versus extracorporeal shockwave lithotripsy for tough bile duct stones, Gastrointes Endosc forty seven:327�334, 1998. Osanai M, et al: Peroral video cholangioscopy to consider indetermi nate bile duct lesions and preoperative mucosal cancerous extension: a prospective multicenter study, Endoscopy 45(8):635�642, 2013. Park do H, et al: Covered versus uncovered wallstent for malignant extrahepatic biliary obstruction: a cohort comparative evaluation, Clin Gastroenterol Hepatol 4(6):790�796, 2006. Piraka C, et al: Transpapillary cholangioscopy directed lithotripsy in patients with troublesome bile duct stones, Clin Gastroenterol Hepatol 5:1333�1338, 2007.
Allopurinol 300 mg generic without a prescription
However gastritis aguda cheap 300 mg allopurinol mastercard, it must be confused strongly that as a end result of the cholangiographic appearance of many biliary illnesses could additionally be indistinguishable gastritis y dolor de espalda 300 mg allopurinol generic overnight delivery, biopsy is often required to rule out malignancy or to verify suspected analysis. Bile Leaks Bile leaks are seen as websites of free extravasation of contrast agent at a site of bile duct injury. Usually two or three ducts drain most commonly into the best posterior sectoral duct, proper hepatic duct, or left hepatic duct (Healey & Schroy, 1953). The recognizable caudate ducts are normally a quantity of centimeters long and drain downward or to the proper. The left hepatic duct (average length, 17 mm) is significantly longer than the proper hepatic duct (average size, 9 mm) and has a longer extrahepatic course. These figures are higher than the true duct dimensions due to some distension produced by direct cholangiography, together with appreciable magnification occurring on any fluoroscopic "spot film. Filling Defects Air Bubbles, Blood Clots, Calculi, Primary and Secondary Bile Duct Cancers, and Parasitic Diseases Air bubbles, though confusing, mostly declare themselves by their perfectly round shape and their distribution to nondependent buildings. Calculous illness (see Chapters 36 and 39) remains the most common filling defect within the biliary system. Other malignancies, including melanoma and intraductal metastases, such as colon most cancers, are additionally extra unusual causes of cholangiographic filling defects (Riopel, 1997). Parasitic infections, corresponding to hydatid disease (see Chapter 74) and infections with Ascaris lumbricoides or Clonorchis sinensis (see Chapter 45), are diseases with worldwide distribution that may also present cholangiographically as intraductal filling defects. A proportion of hepatic hydatid cysts (5% to 10%) rupture into the bile ducts and will simulate choledocholithiasis. Calcified cysts are easy to acknowledge on radiographs, and daughter cysts may cause biliary obstruction. The mucin leads to enlargement of the frequent bile duct beneath the tumor and seems as strandlike filling defects. Ascaris lumbricoides is a generally seen helminth with a prevalence of 90% in some parts of Africa and Asia (see Chapter 45). If the worm passes through the sphincter of Oddi, it could cause acute pancreatitis or a cholestasis syndrome (Winters et al, 1984). In the acute stage, the worm sometimes may be found and extracted from the ampulla, and it can be detected in the biliary tract by cholangiography. The prevalence of this illness has been estimated to be 60% of the final inhabitants of Hong Kong, primarily based on stool ova examinations. Other frequent cholangiographic findings embody broadly dilated extrahepatic bile ducts, which are full of biliary sludge and stones, and intrahepatic duct strictures, which are predominantly discovered within the branches of the left hepatic duct (Yellin & Donovan, 1981). Naval and colleagues (1984) reported profitable endoscopic biliary lavage to eliminate the eggs. Invasion of Fasciola hepatica into the biliary tract also might trigger severe lesions (see Chapter 45). The capacity to visualize the whole biliary tree, the bile duct wall, and other buildings apart from the bile duct lumen increases the diagnostic accuracy and medical utility of those noninvasive strategies, which have turn out to be the gold commonplace for cholangiography. Direct cholangiography is usually reserved for clinical eventualities involving concomitantly planned therapeutic interventions. Akbar A, et al: Rectal nonsteroidal anti-inflammatory medication are superior to pancreatic duct stents in stopping pancreatitis after endoscopic retrograde cholangiopancreatography: a community meta-analysis, Clin Gastroenterol Hepatol 11:778�783, 2013. Working get together report to the World Congress of Gastroenterology, Sydney, J Gastroenterol Hepatol 6:23�24, 1991. Burckhardt H, M�ller W: Verusche �ber die Puncktion der Gallenblase und ihre R�ntgendarstellung, Dtsch Chir 162:168, 1921. Classen M, Demling L: Hazards of endoscopic retrograde cholangiopancreatography, Acta Hepatogastroenterol 22:1�3, 1975. Cottone M, et al: Endoscopic retrograde cholangiography in hepatic hydatid disease, Br J Surg sixty six:107, 1978. Dyrszka H, Sanghavi B: Hepatic hydatid illness: findings on endoscopic retrograde cholangiography, Gastrointest Endosc 29:248�249, 1983. Fukuda Y, et al: Diagnostic utility of peroral cholangioscopy for various bile-duct lesions, Gastrointest Endosc 62(3):374�382, 2005. Glenn F, et al: Percutaneous transhepatic cholangiography, Ann Surg 156:451, 1962. Goldberg E, et al: Pancreatic-duct stent placement facilitates tough frequent bile duct cannulation, Gastrointest Endosc 62(4):592�596, 2005. Huard P, Do-Xuan-Hop ��: La ponction transhepatique des canaux biliares, Bull Soc Med Chir Indochine 15:1090, 1937. Itoi T, et al: Diagnostic peroral video cholangioscopy is an accurate diagnostic software for patients with bile duct lesions, Clin Gastroenterol Hepatol 8(11):934�938, 2010. Jain S, et al: Percutaneous transhepatic cholangiography utilizing the "Chiba" needle: eighty circumstances, Br J Radiol 50:175�180, 1977. Kapral C, et al: Case volume and outcome of endoscopic retrograde cholangiopancreatography: results of a nationwide Austrian benchmarking project, Endoscopy 40(8):625�630, 2008. Karamanolis G, et al: A potential cross-over research utilizing a sphincterotome and a guidewire to enhance the success fee of common bile duct cannulation, World J Gastroenterol 11(11):1649�1652, 2005. Kasugai T, et al: Fiberduodenoscopy: evaluation of 353 examinations, Gastrointest Endosc 18:9�16, 1971. Katsinelos P, et al: Treatment of a duodenal perforation secondary to an endoscopic sphincterotomy with clips, World J Gastroenterol 11: 6232�6234, 2005. Miller G, et al: the use of imaging within the analysis and staging of hepatobiliary malignancies, Surg Oncol Clin N Am 16(2):343�368, 2007. Naval F, et al: Endoscopic biliary lavage in a case of Clonorchis sinensis, Gastrointest Endosc 30:292�294, 1984. Niederau C, et al: Comparison of the extrahepatic bile duct dimension measured by ultrasound and by totally different radiographic methods, Gastroenterology 87:615�621, 1984. Ogoshi K, et al: Endoscopic remark of the duodenum and pancreatocholedochography utilizing duodenofiberscope underneath direct vision, Gastrointest Endosc 12:83�96, 1970. Ohto M, Tsuchiya Y: Non-surgically obtainable percutaneous transhepatic cholangiography: technique and circumstances, Medicina (Tokyo) 6: 735�739, 1969. Okuno M, et al: Changes in serum levels of pancreatic isoamylase, lipase, trypsin, and elastase after endoscopic retrograde pancreatography, Hepatogastroenterology 32:87�90, 1985. Osanai M, et al: Peroral video cholangioscopy to consider indeterminate bile duct lesions and preoperative mucosal cancerous extension: a potential multicenter examine, Endoscopy 45(8):635�642, 2013. Pereiras R Jr, et al: Percutaneous transhepatic cholangiography with the "skinny" needle: a speedy, simple, and accurate methodology within the diagnosis of cholestasis, Ann Intern Med 86:562�568, 1977. In Henning H, editor: Fortschritte der gastroenterologischen Endoskopie, Grafelfing, 1985, Demeter Verlag, pp 124�129. Romagnuolo J, et al: Magnetic resonance cholangiopancreatography: a meta-analysis of test efficiency in suspected biliary illness, Ann Intern Med 139:547�557, 2003.
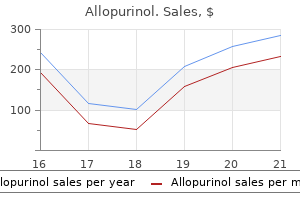
300 mg allopurinol visa
Despite these tips gastritis symptoms upper right quadrant pain discount 300 mg allopurinol amex, antimicrobial prophylaxis specifically for pancreatic resections has not been properly evaluated when it comes to the precise agent to use and its length gastritis diet ������� cheap allopurinol 300 mg amex. Donald and colleagues (2013) recommend that guideline-recommended antimicrobial prophylaxis may not be appropriate for patients undergoing pancreaticoduodenectomy. They present an argument for broadening perioperative antibiotic coverage with the use of piperacillin-tazobactam. Sourrouille and colleagues (2013) suggest a 5 day course of postoperative antimicrobial prophylaxis for sufferers present process pancreaticoduodenectomy. Our follow is to administer one dose of ertapenem preoperatively for causes previously mentioned within the part "Hepatic Resection. Much of that morbidity stems from the robust relationship between intraabdominal infectious problems and the presence of a pancreatic fistula. Behrman and colleagues (2008) retrospectively studied 196 pancreatectomy sufferers with an goal to determine danger elements for intraabdominal sepsis. Approximately 16% of those sufferers developed an infected intraabdominal fluid assortment, and overt pancreatic fistula in addition to soft pancreatic remnant had been discovered to be statistically important factors related to its improvement. The authors also noticed that contaminated fluid collections could occur relatively early within the postoperative course, and surgeons should have a low threshold to image and drain these collections, many of which were polymicrobial in nature. Limongelli etal,2007 Correlationbetween preoperativebiliarydrainage, bileductcontamination,and postoperativeoutcomesfor pancreaticsurgery Prospective collection, retrospective evaluation 220 Toexaminetherelationship betweenpreoperative biliarydrainage, intraoperativebileculture, andpostoperative morbidityandmortalityin patientsundergoing pancreaticsurgery Pancreaticoduodenectomy, totalpancreatectomy, andbiliarybypass Lermiteetal, 2008 Effectofpreoperative endoscopicbiliarydrainage oninfectiousmorbidityafter pancreatoduodenectomy:a case-controlstudy Prospective collection, retrospective analysis 124 Toreporttheinfluenceof preoperativeendoscopic biliarydrainageon postoperativeinfectious morbidityinpatients undergoing pancreaticoduodenectomy Pancreaticoduodenectomy Sivarajetal, 2010 Isbactibiliaapredictorofpoor outcomeof pancreaticoduodenectomy In this report, 138 sufferers present process an operation for obstructive jaundice had both their intraoperative bile and all postoperative infectious complications cultured. Of those 91 patients with bactibilia, 69 had undergone preoperative biliary stenting and 22 had not. Pancreatic fistula was clearly the strongest danger issue for organ/space infection. Schmidt and colleagues (2009) studied preoperative and perioperative risk factors for the development of a pancreatic fistula in pancreaticoduodenectomy patients. First, they confirmed the notion that sufferers in whom a pancreatic fistula develops have a better rate of postoperative wound infection and intraabdominal abscess. Second, they identified a number of operative danger factors for the event of pancreatic fistula. Their multivariate analysis confirmed that an invaginated pancreatic anastomosis and closed suction intraperitoneal drainage were predictive of a pancreatic fistula, whereas persistent pancreatitis and preoperative biliary stenting had been protecting of a pancreatic fistula. Despite these findings, a latest review (Schoellhammer et al, 2014) instructed that no one pancreatic anastomosis is superior and that extra studies are wanted to identify the most effective anastomotic approach. A latest randomized trial studied pasireotide as a attainable adjunct to prevent postoperative pancreatic fistula (Allen et al, 2014). The authors randomly assigned 300 patients present process both pancreaticoduodenectomy or distal pancreatectomy to either perioperative pasireotide or placebo. The main end level was the incidence of pancreatic fistula, leak, or abscess of grade 3 or higher. This finish level was considerably lower in these sufferers handled with pasireotide (9% vs. The authors concluded that this perioperative medication decreases the rate of clinically signifi- cant postoperative fistula, leak, or abscess in sufferers present process pancreatic resection. Regarding distal pancreatectomy particularly, Hamilton and colleagues (2012) performed a randomized controlled trial examining the efficacy of mesh-reinforced stapled closure of the distal pancreas. The authors randomly assigned 54 sufferers to mesh reinforcement and 46 patients to nonmesh reinforcement, in which the first outcome was clinically important pancreatic leak. Other operative danger components contributing to postoperative infectious morbidity after pancreatic resection include longer operative times (Ball et al, 2010; Procter et al, 2010; Sudo et al, 2014; Sugiura et al, 2012; Wang et al, 2007) and need for perioperative blood transfusion (Ball et al, 2010) (see Table 12. Their multivariate analysis instructed that increased operative length is an unbiased risk issue for infectious complications and hospital size of keep. Their examine involved 4817 sufferers and determined that longer operative instances were associated with each morbidity and mortality. This led the authors to suggest blood transfusion and operative time as quality indicators for pancreaticoduodenectomy. This most up-to-date research randomized 137 sufferers undergoing pancreaticoduodenectomy. The examine was stopped early because of the reality that there was a substantial distinction in mortality between the 2 groups. The drained patients had a mortality of 3%, whereas the undrained group skilled a 12% mortality fee. Beyond this, pancreaticoduodenectomy with out intraperitoneal drainage was considerably associated with a rise in the number of problems per affected person, an increase within the variety of patients who had no less than one complication rated at grade 2 or higher, and a higher average issues severity. From an infectious standpoint, pancreaticoduodenectomy without intraperitoneal drainage was related to a higher price of intraabdominal abscess (25% vs. This examine subsequently provides strong evidence supporting the position of intraperitoneal drains on the time of pancreaticoduodenectomy. Taken within the context of other up to date literature on this topic, the best method to peritoneal drainage remains unclear and ought to be individualized to the precise patient. If positioned on the time of pancreaticoduodenectomy, the timing of drain elimination can be controversial. Recent prospective studies, together with a randomized trial, have advised that early drain removing based mostly on drain amylase levels can decrease the rate of postoperative problems, together with infectious ones (Bassi et al, 2010; Kawai et al, 2006). To summarize, risk mitigation at the operative degree for a pancreaticoduodenectomy or distal pancreatectomy consists of the efficient efficiency of the operation using cautious operative method in an effort to avoid pointless blood loss. The pancreaticoenteric anastomosis throughout pancreaticoduodenectomy is still performed in accordance with surgeon desire but should be done meticulously. With regard to distal pancreatectomy, stapled closure of the pancreas with bioabsorbable mesh buttress seems promising in the prevention of pancreatic fistula. Perioperative administration of pasireotide has demonstrated efficacy in decreasing pancreatic fistula after pancreaticoduodenectomy and distal pancreatectomy. The use of intraperitoneal drains and the timing of their removing stay controversial. Postoperative Risk Mitigation Postoperative blood glucose control is essential after surgical procedures and has an impression on affected person outcomes, as discussed earlier. Synbiotic remedy has proven some promising results in mitigating infectious problems in hepatic resection sufferers (see part "Hepatic Resection"). Rayes and colleagues (2007) carried out a randomized, double-blind trial to consider the potential advantage of synbiotic therapy in patients undergoing pancreaticoduodenectomy with preservation of the pylorus. All patients were began on enteral diet instantly postoperatively through a nasojejunal tube positioned at the time of the operation. The experimental group received enteral vitamin plus synbiotics, whereas the management group received enteral diet plus placebo. Ambiru S, et al: Poor postoperative blood glucose management increases surgical website infections after surgical procedure for hepato-biliary-pancreatic cancer: a prospective study in a high-volume institute in Japan, J Hosp Infect 68(3):230�233, 2008. The Veterans Affairs Total Parenteral Nutrition Cooperative Study Group, N Engl J Med 325(8):525�532, 1991. American Society of Health-System Pharmacists, Am J Health Syst Pharm 56(18):1839�1888, 1999.
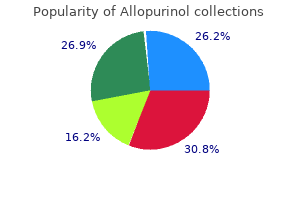
Cheap 300 mg allopurinol visa
Unresectable disease was discovered on the time of laparoscopy in eighty four cases gastritis vs pregnancy symptoms 300 mg allopurinol mastercard, for an general incidence of 21% gastritis diet advice discount 300 mg allopurinol with amex. Sixty-nine patients had unresectable illness recognized throughout open exploration, for an overall false-negative price of 22%. This high false-negative fee was attributed primarily to failure to establish lymph node metastases or to detect vascular invasion. Laparoscopic staging can be utilized within the evaluation of colorectal metastases (Rahusen et al, 1999) (see Chapter 92). Approximately one half of all sufferers with new diagnoses of colorectal cancer will subsequently develop liver metastases, yet solely 20% are candidates for curative hepatic resection. Most authors agree that hepatic cirrhosis, extrahepatic tumor spread, and vital bilobar disease are relative contraindications for hepatic resection. Of these in whom resection was considered impossible, 18 had been untreatable altogether, and 28 patients had different treatments. Using such a risk scoring system to help guide the addition of laparoscopy to higher-risk patients ought to enhance the general yield from laparoscopy. A minority of sufferers (20% to 35%) with pancreatic and periampullary malignancies (see Chapters 62 and 63) are suitable candidates for curative resection (Conlon & Brennan, 2000; Conlon & Minnard, 1997; Jimenez et al, 2000). Imaging studies can predict resectability in 57% to 88% of circumstances (Contreras et al, 2009; Freeny, 2001; Mayo et al, 2009; Pisters et al, 2001). The Society of Surgical Oncology tips from the 2009 consensus assertion regarding the pretreatment evaluation of pancreatic cancer state the following relating to using laparoscopy: 1. In this report, laparoscopic examinations demonstrated that forty two (57%) of 73 sufferers had unresectable illness, primarily due to peritoneal or omental metastases. Since these early papers, laparoscopy has been refined and is now similar to open exploration in defining resectability. Reddy and associates (1999) confirmed these findings in a later report; 29% had been spared additional intervention. Sonography was particularly useful in figuring out venous (42%) and arterial (38%) involvement, which precludes curative resection. In a evaluation of 1045 sufferers with imaging-determined pancreatic and peripancreatic tumors, 12% of sufferers with pancreatic tumors had findings on diagnostic laparoscopy that precluded resection. The yield was larger for patients diagnosed with pancreatic adenocarcinoma and less for patients with tumors of the ampulla, distal bile duct, duodenum, and neuroendocrine tumors. In addition to the advantages associated to restoration from laparoscopy, a quantity of authors have found that the laparoscopic strategy to staging may be superior to the open exploration for the detection of occult metastases (Shoup et al, 2004). This is set partially by the kind of malignancy (Brooks et al, 2002; Vollmer et al, 2002). The relative yield of diagnostic laparoscopy may be lower at facilities that have an aggressive palliative surgical approach, whereas even if a disease is unresectable, laparotomy is performed regardless for palliative intervention with bypass. Friess H, et al: the position of diagnostic laparoscopy in pancreatic and periampullary malignancies, J Am Coll Surg 186:675�682, 1998. Gouillat C, et al: Value of intraoperative ultrasonography within the surgical therapy of malignant tumors, Ann Chir forty five:534�539, 1992. Gozzetti G, et al: Intraoperative ultrasonography in surgical procedure for liver tumors, Surgery 99:523�529, 1986. Jakimowicz J: Review: intraoperative ultrasonography during minimal entry surgery, J R Coll Surg Edinb 38:231�238, 1993. Jeffers L, et al: Laparoscopically directed fantastic needle aspiration for the diagnosis of hepatocellular carcinoma: a safe and correct method, Gastrointest Endosc 34:235�237, 1988. Machi J, et al: Laparoscopic ultrasonography versus operative cholangiography throughout laparoscopic cholecystectomy: evaluation of the literature and a comparison with open intraoperative ultrasonography, J Am Coll Surg 1999:360�367, 1999. Makuuchi M, et al: Intraoperative ultrasonic examination for hepatectomy, Jpn J Clin Oncol eleven:367�372, 1981. Andren-Sandberg A, et al: Computed tomography and laparoscopy in the assessment of the affected person with pancreatic cancer, J Am Coll Surg 186:35�40, 1998. Belghiti J, et al: Surgical remedy of hepatocellular carcinoma in cirrhosis: worth of preoperative ultrasonography, Gastroenterol Clin Biol 10:244�247, 1986. Bismuth H, Castaing D: �chographie per-op�ratoire du foie et des voies biliaires, Paris, 1985, Blammarion. Bismuth H, et al: the use of operative ultrasound in surgery of main liver tumors, World J Surg 11:610�614, 1987. Bloed W, et al: Role of intraoperative ultrasound of the liver with improved preoperative hepatic imaging, Eur J Surg 166:691�695, 2000. Catheline J, et al: A comparison of laparoscopic ultrasound versus cholangiography in the evaluation of the biliary tree during laparoscopic cholecystectomy, Eur J Ultrasound 10:1�9, 1999. Charfare H, Cheslyn-Curtis S: Selective cholangiography in 600 patients undergoing cholecystectomy with 5-year follow-up for residual bile duct stones, Ann R Coll Surg Engl 85:167�173, 2003. Conlon R, et al: the worth of intraoperative ultrasound throughout hepatic resection in contrast with improved preoperative magnetic resonance imaging, Eur J Ultrasound sixteen:211�216, 2003. In Cuschieri A, Berci G, editors: Common bile duct exploration, Boston, 1984, Martinus Nijhoff, pp 55�59. Decker G, et al: One hundred laparoscopic choledochotomies with major closure of the frequent bile duct, Surg Endosc 17:12�18, 2003. Dobronte Z, et al: Rapid growth of malignant metastases within the stomach wall after laparoscopy, Endoscopy 10:127�130, 1978. Nagasue N, et al: Intraoperative ultrasonography for the surgical therapy of hepatic tumors, Acta Chir Scand one hundred fifty:311�316, 1984. Nickkholgh A, et al: Routine versus selective intraoperative cholangiography throughout laparoscopic cholecystectomy: a survey of two,a hundred thirty patients throughout laparoscopic, Surg Endosc 20:868�874, 2006. Nugent N, et al: Low incidence of retained widespread bile duct stones utilizing a selective policy of biliary imaging, Surgeon three:352�356, 2005. Sarli L, et al: Scoring system to predict asymptomatic choledocholithiasis earlier than laparoscopic cholecystectomy: a matched case-control research, Surg Endosc 17:1396�1403, 2003a. Sarli L, et al: Preoperative endoscopic sphincterotomy and laparoscopic cholecystectomy for the management of cholecystocholedocholithiasis: 10-year experience, World J Surg 27:180�186, 2003b. Shoup M, et al: Port-site metastasis after diagnostic laparoscopy for upper gastrointestinal tract malignancies: an unusual entity, Ann Surg Oncol 9:632�636, 2002. Shoup M, et al: Is there a role for staging laparoscopy in sufferers with locally superior, unresectable pancreatic adenocarcinoma Sigel B, et al: Comparative accuracy of operative ultrasonography and cholangiography in detecting widespread duct calculi, Surgery 94:715� 720, 1983. Siperstein A, et al: Comparison of laparoscopic ultrasonography and fluo-rocholangiography in 300 sufferers present process laparoscopic cholecystectomy, Surg Endosc thirteen:113�117, 1999. Thaler K, et al: the evolving position of staging laparoscopy in the remedy of colorectal hepatic metastasis, Arch Surg a hundred and forty:727�734, 2005. Tokumura H, et al: Laparoscopic management of common bile duct stones: transcystic strategy and choledochotomy, J Hepatobiliary Pancreat Surg 9:206�212, 2002. Torzilli G, et al: Ultrasound-guided liver resections for hepatocellular carcinoma, Hepatogastroenterology 49:21�27, 2002. Velanovich V: the effects of staging laparoscopy on trocar site and peritoneal recurrence of pancreatic most cancers, Surg Endosc 18:310�313, 2004. Weitz J, et al: Selective use of diagnostic laparoscopy prior to planned hepatectomy for sufferers with hepatocellular carcinoma, Surgery one hundred thirty five:273�281, 2004.
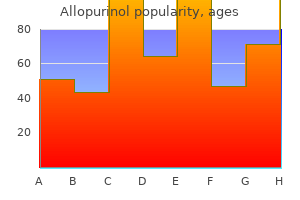
300 mg allopurinol otc
Continuous epidural analgesia is incessantly averted because of issues about coagulopathy gastritis cancer generic allopurinol 300 mg fast delivery, thrombocytopenia gastritis journal articles 300 mg allopurinol fast delivery, and the elevated risk of hematoma. In a small sequence, patient-controlled analgesia has been discovered to be a secure and effective technique of managing ache after hepatic resection (Roy et al, 2006). Propofol is a extra sensible choice than benzodiazepines for sedation because of its shorter recovery time, which can enable extra reliable serial neurologic assessment (Khamaysi et al, 2011). Nonsteroidal antiinflammatory brokers ought to be used sparingly due to the potential for peptic ulceration, fluid retention from inhibition of renal prostaglandin synthesis, precipitation of hepatorenal syndrome, and bleeding because of antiplatelet activity, gastrointestinal irritation, and renal failure (Bosilkovska et al, 2012; Dwyer et al, 2014). Hepatic encephalopathy warrants evaluation and remedy of infections and administration of oral lactulose or lactitol suppository (Wright & Jalan, 2007). Second-line agents for the remedy of hepatic encephalopathy embrace oral antibiotics similar to neomycin, metronidazole, and rifaximin (Al Sibae & McGuire, 2009). Early enteral vitamin is advocated after liver resection because of a perceived decrease in postoperative issues (Richter et al, 2006). Compared with enteral nutrition, parenteral vitamin for 7 days before deliberate hepatectomy in patients with liver cirrhosis and continued for 7 days afterward was related to fewer septic problems and a lower mortality fee (Fan et al, 1994). In reality, the benefits and really helpful route of dietary help after hepatopancreatobiliary surgery are debatable due to conflicting results from a couple of randomized trials and systematic evaluation (Fan et al, 1994; Koretz et al, 2012). At present, no specific pointers or suggestions are available, even throughout liver regeneration or in situations of acute pancreatitis (Poropat et al, 2015). Postoperative Care after Pancreaticoduodenectomy Postoperative complications of the Kausch-Whipple process, similar to anastomotic leak, fistula, and stomach collections, are relatively frequent and range with the sort of pancreaticoenteric anastomosis, pancreatic texture and intraoperative blood transfusion (Fathy et al, 2008) (see Chapters 27 and 66). Surgical exploration and prognosis are often dictated by the degree of destruction and inflammation of the retroperitoneum (Ho et al, 2005). Prophylactic octreotide has no impact on the charges of pancreatic fistula or total problems after pancreaticoduodenectomy (Yeo et al, 2000). However, the perioperative use of pasireotide was related to vital decrease in postoperative pancreatic fistula, leak, or abscess (Allen et al, 2014). Venous Thromboembolism Prophylaxis Compared with the final population, patients with cirrhosis are at higher threat of bleeding due to anemia, thrombocytopenia, and the inability of the liver to produce procoagulants in response to the stress of bleeding. Yet these sufferers handle to strike a fine balance between prothrombotic and anticoagulating proteins and different endogenous products (Senzolo et al, 2009). Severe thrombocytopenia rather than coagulopathy is essentially the most vital risk factor for bleeding after invasive procedures (Giannini et al, 2010; Rockey et al, 2009). Failure to develop hypophosphatemia is a marker of postoperative hepatic insufficiency and mortality (Squires et al, 2014). Liver regeneration is a protracted compensatory process of hepatocytes replication that can be assessed by magnetic resonance spectroscopic imaging (Fausto et al, 2006; Zakian et al, 2005) (see Chapter 6). Early postoperative hyperglycemia after pancreaticoduodenectomy increases the risk of infectious issues, delayed gastric emptying, and reoperation (Eshuis et al, 2011). Alessandria C, et al: Noradrenalin vs terlipressin in patients with hepatorenal syndrome: a prospective, randomized, unblinded, pilot study, J Hepatol 47(4):499�505, 2007. Angeli P, Merkel C: Pathogenesis and management of hepatorenal syndrome in patients with cirrhosis, J Hepatol 48(Suppl 1):S93� S103, 2008. Appenrodt B, et al: Prevention of paracentesis-induced circulatory dysfunction: midodrine vs albumin. Arroyo V, et al: Definition and diagnostic criteria of refractory ascites and hepatorenal syndrome in cirrhosis. Arvaniti V, et al: Infections in sufferers with cirrhosis improve mortality four-fold and should be utilized in figuring out prognosis, Gastroenterology 139(4):1246�1256. Bahirwani R, et al: Factors that predict short-term intensive care unit mortality in patients with cirrhosis, Clin Gastroenterol Hepatol 11(9):1194�1200. Balzan S, et al: the "50-50 criteria" on postoperative day 5: an accurate predictor of liver failure and dying after hepatectomy, Ann Surg 242(6):824�828, dialogue 828-829, 2005. Bambha K, et al: Predictors of early re-bleeding and mortality after acute variceal haemorrhage in patients with cirrhosis, Gut 57(6):814� 820, 2008. Berendes E, et al: Effects of enflurane and isoflurane on splanchnic oxygenation in humans, J Clin Anesth 8(6):456�468, 1996. Berzigotti A, et al: Elastography, spleen size, and platelet count determine portal hypertension in patients with compensated cirrhosis, Gastroenterology 144(1):102�111. Bosilkovska M, et al: Analgesics in sufferers with hepatic impairment: pharmacology and scientific implications, Drugs 72(12):1645�1669, 2012. Braga M, et al: A prognostic score to predict major issues after pancreaticoduodenectomy, Ann Surg 254(5):702�707, dialogue 707-708, 2011. Bureau C, et al: Transient elastography precisely predicts presence of great portal hypertension in patients with persistent liver illness, Aliment Pharmacol Ther 27(12):1261�1268, 2008. Cazzaniga M, et al: the systemic inflammatory response syndrome in cirrhotic patients: relationship with their in-hospital end result, J Hepatol 51(3):475�482, 2009. Cholongitas E, et al: Risk elements, sequential organ failure evaluation and mannequin for end-stage liver illness scores for predicting brief time period mortality in cirrhotic patients admitted to intensive care unit, Aliment Pharmacol Ther 23(7):883�893, 2006. De Goede B, et al: Morbidity and mortality associated to non-hepatic surgery in patients with liver cirrhosis: a scientific review, Best Pract Res Clin Gastroenterol 26(1):47�59, 2012. Delco F, et al: Dose adjustment in sufferers with liver illness, Drug Saf 28(6):529�545, 2005. Demetriades D, et al: Liver cirrhosis in patients undergoing laparotomy for trauma: effect on outcomes, J Am Coll Surg 199(4):538�542, 2004. Elkrief L, et al: Diabetes mellitus is an independent prognostic issue for major liver-related outcomes in patients with cirrhosis and persistent hepatitis C, Hepatology 60(3):823�831, 2014. Fathy O, et al: 216 circumstances of pancreaticoduodenectomy: risk elements for postoperative problems, Hepatogastroenterology 55(84):1093� 1098, 2008. Fauconnet P, et al: Hepatopulmonary syndrome: the anaesthetic issues, Eur J Anaesthesiol 30(12):721�730, 2013. Fayad L, et al: the efficiency of prognostic models as predictors of mortality in patients with acute decompensation of cirrhosis, Ann Hepatol 14(1):83�92, 2015. Fenger-Eriksen C, et al: Fibrinogen focus substitution remedy in sufferers with huge haemorrhage and low plasma fibrinogen concentrations, Br J Anaesth 101(6):769�773, 2008. Fernandez J, et al: Primary prophylaxis of spontaneous bacterial peritonitis delays hepatorenal syndrome and improves survival in cirrhosis, Gastroenterology 133(3):818�824, 2007. Ferral H, et al: Survival after elective transjugular intrahepatic portosystemic shunt creation: prediction with model for end-stage liver disease score, Radiology 231(1):231�236, 2004. Franzetta M, et al: Prognostic components of cirrhotic sufferers in extrahepatic surgery, Minerva Chir 58(4):541�544, 2003. Georgiou C, et al: Cirrhosis and trauma are a deadly combination, World J Surg 33(5):1087�1092, 2009. Gupta D, et al: Pulmonary perform changes after large volume paracentesis, Trop Gastroenterol 21(2):68�70, 2000. Harimoto N, et al: Significance of stroke volume variation during hepatic resection under infrahepatic inferior vena cava and portal triad clamping, Fukuoka Igaku Zasshi 104(10):362�369, 2013.
Snake Butter (Shiitake Mushroom). Allopurinol.
- Reducing high cholesterol and other conditions.
- Prostate cancer.
- Dosing considerations for Shiitake Mushroom.
- How does Shiitake Mushroom work?
- Are there safety concerns?
- What is Shiitake Mushroom?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96669
Allopurinol 300 mg buy discount on line
It was not till the introduction of the laparoscopic cholecystectomy in the late Eighties that the function for an associated less invasive method of treating choledocholithiasis became a precedence gastritis symptoms lump in throat generic allopurinol 300 mg on line. In addition gastritis symptoms during pregnancy cheap allopurinol 300 mg fast delivery, the capability and expertise of the obtainable personnel will have an result on the therapy algorithm. The commonest medical eventualities encountered by surgeons embody known or suspected stones prior to cholecystectomy, the analysis of stones intraoperatively, and stones recognized subsequent to cholecystectomy. In most patients, our preferred technique is laparoscopic cholecystectomy with selective intraoperative cholangiogram (see Chapter 23). This allows for each clearance of the bile duct and evaluation of further or various pathologies, similar to impacted stones, strictures, or malignancy. In both cholangitis and pancreatitis, as quickly as the patient has sufficiently recovered, cholecystectomy ought to be accomplished throughout the same hospitalization as early recurrence of symptoms is widespread, and may result in vital morbidity (Chang et al, 2000; Li et al, 2010). Similarly, if stone extraction fails as a outcome of the dimensions of the stones, laparoscopic exploration is an affordable next step. Transcystic exploration is usually performed utilizing a normal laparoscopic cholecystectomy trocar configuration. When the probability of endoscopic clearance is questionable or low, we proceed with a transcholedochal exploration. The first and best step in facilitating passage of stones by way of the ampulla is pharmacologic rest of the sphincter of Oddi by utilizing glucagon (Petelin, 1993). After giving 1 mg of intravenous glucagon and ready 3 minutes, the duct is vigorously irrigated with saline or contrast in an try and flush the stones via the ampulla (Ponce et al, 1989). This approach is most successful for sludge and stones less than 4 mm (Kroh & Chand, 2008). If flushing is unsuccessful, two additional methods are used: dilation of the ampulla and choledochoscopy. Ampullary dilation is performed by passing a wire via the cystic duct and into the duodenum beneath fluoroscopic guidance. A 4- to 6-mm diameter, 4-cm long ureteral balloon is superior over the wire and positioned throughout the ampulla. Some surgeons choose to proceed straight to choledochoscopy without trying ampullary dilation because it allows direct visualization of the bile duct and stones. Once the stones are recognized, they can be gently pushed by way of the ampulla with the tip of the cholangioscope, or they can be snared. To snare the stones, we suggest a helical stone retrieval basket, which is passed via the working channel of the cholangioscope. Some authors suggest blind or fluoroscopically guided wire basket stone seize and extraction; in our experience, this has confirmed less successful and has a better danger of harm. Large stones which are delicate, can often be crushed by tightening the snare around them, and the debris can then be snared individually or pushed by way of the ampulla into the duodenum. For large stones which would possibly be too onerous to crush, a laser or mechanical lithotripsy catheter can be handed by way of the cholangioscope to fracture the stone beneath direct visualization. Finally, in bile ducts with significant irritation or strictures, a biopsy must be considered. Malignancy may be an inciting occasion in the growth of ductal debris or ductal obstruction. The success rate of a laparoscopic transcystic method to choledocholithiasis by experienced surgical groups is 80% to 90% (Kroh & Chand, 2008). Occasionally, the cystic duct inserts into the very distal widespread duct or at an acute angle, making entry to the proximal frequent duct difficult. Large stones, impacted stones, and significant inflammation can all increase the issue of transcystic bile duct clearance. Laparoscopic choledochotomy is indicated when the transcystic method fails or within the presence of a quantity of, large, or impacted stones. Gallstones and Gallbladder Chapter 36B Stones within the bile duct: minimally invasive surgical approaches 607 duodenum and mobilizing the duodenum down to the extent of the pancreas. Stones could also be flushed out of the ductotomy, removed immediately with atraumatic graspers, or extracted utilizing a snare passed by way of the cholangioscope as described within the transcystic strategy. There is a mechanical advantage to eradicating impacted stones directly by way of a choledochotomy, though stones impacted in the head of the pancreas may require a transduodenal method. After clearance of the duct and completion of the exploration, the ductotomy is closed primarily or often over a T-tube. Historically, T-tubes have been used to decompress the biliary tree and had been thought to reduce bile leaks. T-tubes, nevertheless, have potential morbidity, including inadvertent displacement, erosion, cholangitis, nutritional deficiencies from bile loss (Gurusamy et al, 2013). Our choice is to shut the ductotomy with easy interrupted sutures, spaced evenly to keep away from duct ischemia. If a T-tube is used, the ductotomy is closed across the base of the tube by utilizing a couple of sutures adjoining to the facet of the T-tube, and the tube is exteriorized by way of a lateral trocar website. A ultimate cholangiogram by way of the T-tube is carried out on the conclusion of the case. Tubes are left in place for three weeks to promote formation of an inflammatory tract around the tube. The T-tube can then be gently removed, and the tract will collapse and seal spontaneously. If stones are discovered postoperatively, percutaneous stone extraction by way of the T-tube is profitable in 95% of cases (Burhenne, 1980). The total success price of laparoscopic choledochotomy is 83% to 96%, with a morbidity rate of 5% to 10%, and mortality price of 1% (Verbesey & Birkett, 2008). Major benefits of the transcholedochal method include easier entry to each the higher and lower ductal methods, and extraction of any measurement stones. Conversion to an open process should be thought of in troublesome cases, although difficult laparoscopic cases are regularly additionally challenging open cases; referral to a specialty center should all the time be thought-about earlier than changing to a laparotomy. In sufferers with a high threat of recurrent stone disease or formation of a biliary stricture, due to irritation or a small duct, a definitive bypass should be thought-about. To achieve access to the duodenum, the best colon is mobilized, and a Kocher maneuver is accomplished. With the duodenum elevated, a surgical sponge posterior to the pinnacle of the pancreas could also be useful. This will elevate the duodenum and take up enteric fluids leaking into the sphere once the duodenotomy is created. A longitudinal incision is made within the antimesenteric wall of the second portion of the duodenum with electrocautery or ultrasonic shears, to expose the main duodenal papilla. The two primary options for bypass are choledochoduodenostomy or Roux-en-Y hepaticojejunostomy. Currently, there are insufficient comparative knowledge to recommend one technique of biliary-enteric anastomosis over another (see Chapters 31 and 36A). There are a selection of retrospective research comparing the 2 anastomoses that show equal outcomes and morbidity (Luu et al, 2013; Narayanan et al, 2013; Santore et al, 2011).
Buy allopurinol 300 mg visa
This downside was examined with a recent choice analysis gastritis xarelto allopurinol 300 mg order overnight delivery, utilizing possibilities and outcomes derived from a pooled evaluation of printed research (Kao et al gastritis glutamine purchase 300 mg allopurinol with mastercard, 2005). Kao and colleagues (2005) beneficial prophylactic posttransplantation cholecystectomy for cardiac transplant recipients with asymptomatic cholelithiasis, an approach advocated by different studies as nicely due to the increased morbidity and mortality that has been demonstrated with subsequent pressing or emergent cholecystectomy compared with the overall populace (Kilic et al, 2013). This stays an space of debate, nonetheless, as different research have demonstrated that expectant administration of asymptomatic gallstones is protected (Takeyama, 2006). Asymptomatic gallstones found at an unrelated open gastrointestinal operation ought to prompt a cholecystectomy, if publicity is sufficient and if the operation can be done safely. In contrast, children with asymptomatic gallstones brought on by different etiologies could be safely managed expectantly, and these gallstones have been shown to regress in 17% to 34% of cases (Curro et al, 2007). Finally, gallstones have a proven association with gallbladder carcinoma (Tewari, 2006) (see Chapter 49). In a evaluate of 200 consecutive calculous cholecystitis specimens, AlboresSaavedra and colleagues (1980) reported that 83% exhibited epithelial hyperplasia, 13. In areas endemic for gallbladder most cancers, the chance of carcinoma will increase with larger gallstones: the relative threat rises from 2. Native Americans and sufferers with gallbladder calcification also have the next incidence of gallbladder cancer. Elective cholecystectomy has been really helpful in patients with gallstones greater than three cm in diameter, however no proof is on the market to help that such an approach is warranted from an oncologic standpoint (Gupta et al, 2004; Mohandas et al, 2006; Tewari 2006). Symptomatic Gallstones Approximately 30% of sufferers with gallstones will develop signs, and as quickly as this occurs, cholecystectomy is usually indicated for each symptomatic enchancment and to prevent further issues. The spectrum of severity characterizing symptomatic gallstones ranges from episodic pain to lifethreatening an infection and shock (see Chapters 32 and 33). Biliary colic is the most typical medical presentation of symptomatic gallstones (see Chapter 13). This visceral ache probably reflects the gallbladder contracting against a cystic duct blocked by an impacted gallstone. If pain persists and escalates, it could herald a worse complication of gallstones, such as cholecystitis, cholangitis, or pancreatitis. Pain typically remits after several hours, which can create a false sense of security in some sufferers. More than 60% of patients will suffer recurrent pain inside 2 years of their preliminary assault, and several studies have indicated that gallstoneassociated complications occur more frequently in patients who expertise biliary colic. Acute cholecystitis happens in about 20% of patients with symptomatic gallstones (see Chapter 33). The pathogenesis is prolonged calculous obstruction of the cystic duct with resulting irritation. The inflamed gallbladder becomes dilated and edematous, manifested by wall thickening, and an exudate of pericholecystic fluid can develop. If the gallstones are sterile, the irritation is initially sterile, which may happen in sufferers with cholesterol gallstones. In different instances, nonetheless, gallstone formation happens on account of bacterial colonization of the biliary tree, rendering pigmented gallstones containing bacterial microcolonies (Stewart et al, 2002). Further, no enhance in morbidity is associated with concomitant cholecystectomy (Klaus et al, 2002; Stewart et al, 1989). Studies reported no increase in graft an infection or morbidity when cholecystectomy was performed following closure of the retroperitoneum; however, newer data show related mortality rates with or with out concomitant cholecystectomy. Children with asymptomatic gallstones comprise two major etiologic teams: those with hemolytic anemia (sickle cell illness, -thalassemia, hemoglobinopathies) and those whose cholelithiasis stems from some other cause (total parenteral diet, short bowel syndrome, cardiac surgical procedure, leukemia, lymphoma). Expectant management for youngsters with hemolytic anemia is related to a big improve in morbidity and postoperative hospital keep, and elective cholecystectomy is therefore recommended (Curro et al, 2007). For sufferers with sickle cell disease and asymptomatic gallstones, elective cholecystectomy is suggested as a end result of expectant administration yields more than a twofold improve in morbidity. Further, the analysis of acute cholecystitis can be troublesome to differentiate A. Research on the pathogenesis of gallstone-associated infections has proven that sufferers with bacteria-laden gallstones have extra extreme biliary infections. In addition, acute cholecystitis can coexist with choledocholithiasis, cholangitis, or gallstone pancreatitis. The preliminary remedy for patients with acute cholecystitis is intravenous hydration, antibiotics, and bowel rest. Many sufferers ought to be supplied early cholecystectomy, however others will benefit from delayed intervention, both following conservative remedy or percutaneous gallbladder drainage. One consideration is affected person comorbidity; emergency cholecystectomy in patients with vital comorbidities may be associated with high morbidity (20% to 30%) and mortality (6% to 30%) rates. Guidelines for the management of acute cholecystitis and acute cholangitis have been described at an international consensus meeting held in Tokyo in 2006, and up to date pointers have been then revealed in 2013 (Takada et al, 2007, 2013). The Tokyo Guidelines outline three ranges of severity for acute cholecystitis and function a helpful gizmo within the management of acute cholecystitis (Table 37. Patients presenting with mild grade I acute cholecystitis should be supplied early cholecystectomy, carried out laparoscopically if possible. Several studies have documented excessive success charges for laparoscopic cholecystectomy when the procedure is performed within 72 hours of onset of acute cholecystitis (Hadad et al, 2007; Yamashita et al, 2013). Further, a Cochrane Review of 5 randomized trials confirmed a shorter hospital keep for early cholecystectomy patients and no significant difference in complication rates or conversion charges between early laparoscopic cholecystectomy (within 7 days) versus delayed laparoscopic cholecystectomy (6 to 12 weeks) (Gurusamy & Samraj, 2006). Conversion rates, nevertheless, had been 45% among patients randomized to the delayed group, which required a cholecystectomy between 1 and 6 weeks. For sufferers with important medical issues, cholecystectomy might must be delayed to maximize medical remedy. In these circumstances, laparoscopic cholecystectomy should be performed, if attainable, within 7 days of the acute sickness. In circumstances with severe local inflammation, early gallbladder drainage (percutaneous or surgical) is recommended as the initial treatment of selection, adopted by elective cholecystectomy once the acute inflammation resolves (see Chapters 30 and 34). Several research have correlated such findings as age older than 50 years, male intercourse, presence of diabetes, elevated bilirubin level (>1. Other elements suggestive of a significant inflammatory course of embrace symptoms of gastric outlet obstruction. Mild gallbladder irritation, no organ dysfunction the presence of a number of of the next: 1. Marked local irritation (biliary peritonitis, pericholecystic abscess, hepatic abscess, gangrenous cholecystitis, emphysematous cholecystitis) Associated with dysfunction of any one of many following: 1. Computed tomographic scan demonstrating a extreme inflammatory process in the setting of acute cholecystitis. This patient was treated with percutaneous cholecystostomy, adopted by elective laparoscopic cholecystectomy as soon as the inflammatory process had resolved.
Allopurinol 300 mg generic line
Invasive imaging of the biliary tree with endoscopic or percutaneous cholangiography permits stent placement diabetic gastritis diet 300 mg allopurinol discount overnight delivery, which might facilitate intraoperative identification of right and left hepatic ducts (see Chapters 20 gastritis diet juice allopurinol 300 mg cheap on line, 29, and 30). It can also be important to acknowledge that instrumentation of the biliary tree introduces bacterial contamination that, in a setting of biliary stasis, may end up in cholangitis, periductal irritation, and the next threat of postoperative infections. Caution should even be exercised to avoid percutaneous drainage if it is unlikely that the stent can be passed throughout the obstructing lesion. These complexities underscore the crucial importance of an skilled multidisciplinary staff reviewing and treating advanced biliary obstruction, particularly at the biliary confluence. Depending on the underlying pathology, there are a selection of options for restoration of biliary continuity with the alimentary tract. For instance, choledocholithiasis refractory to local exploration could require choledochoduodenostomy. Other benign etiologies, corresponding to iatrogenic bile duct harm, strictures from earlier biliary-enteric operations, choledochal cysts, or inflammatory strictures, might require restoration with Roux-en-Y choledochojejunostomy or hepaticojejunostomy. Additionally, benign proximal biliary strictures in addition to malignancy (cholangiocarcinoma) could require anastomosis between intrahepatic ducts and jejunum. Finally, the gallbladder may also be utilized to facilitate drainage (cholecystoduodenostomy and cholecystojejunostomy). Although nonoperative measures can be utilized in most conditions, familiarity with the varied surgical strategies can enable applicable restoration of biliary-enteric continuity when the state of affairs calls for (see Chapter 42). Caution must be exercised in the setting of long-standing biliary obstruction or circumstances related to ipsilateral hepatic atrophy and contralateral hypertrophy. In the state of affairs of marked right hemiliver atrophy, the liver hilum and portal buildings will become rotated in a counterclockwise manner. In cases of very profound right liver atrophy, access to the biliary confluence might require a thoracoabdominal incision. Hepaticojejunostomy Despite the necessity for a further anastomosis (at the jejunojejunostomy), Roux-en-Y hepaticojejunostomy is the most common surgical reconstruction for biliary obstruction. The jejunum is usually anastomosed to the frequent hepatic duct just distal to the confluence of the right and left hepatic ducts. Disadvantages embrace necessity for two anastomoses and exclusion of bile from the duodenum. Access to the proper portal pedicle containing the best hepatic duct could be achieved by isolating the pedicle in an extrahepatic location or by exposing the pedicle via intrahepatic dissection. By persevering with this airplane of dissection to the right (onto the cystic plate), the best hepatic duct may be uncovered (Strasberg et al, 2008). If the extrahepatic portion of the right hepatic duct is too short to be visualized in this way (as is commonly the case), the intrahepatic strategy may be used. This requires hepatotomies within the caudate course of simply posterior to the porta hepatis and alongside the bottom of the gallbladder fossa. Incision and Exposure A right subcostal incision with or without an upper midline extension or a left subcostal extension followed by upward elevation and cephalad retraction of the costal margin offers adequate exposure for construction of any biliary-enteric anastomosis. The ligamentum teres is ligated and divided, and the falciform ligament is split to its most cephalad extent on the diaphragm. If direct decompression of the gallbladder is not to be undertaken, cholecystectomy can be advantageous for identification of the cystic duct, which could be dissected to its level of insertion onto the frequent hepatic duct. Cholecystectomy may also expose the cystic plate, which runs in continuity with the hilar plate. Because of its longer extrahepatic course, the left hepatic duct is the preferred target. After ligation of the ligamentum teres with a agency tie, retraction is applied to elevate the left hemiliver. This may be achieved by exposing the biliary drainage of the left hemiliver throughout the umbilical fissure (Blumgart, 1987; Jarnagin et al, 1998; Voyles et al, 1983). If the left hemiliver has not atrophied from long-standing biliary obstruction, unilateral left-sided biliary decompression will successfully relieve obstructive jaundice and restore hepatic function even when the biliary drainage of the excluded right hemiliver remains obstructed. To prepare for biliary-enteric anastomosis, the duct must be dissected free for 1. A defunctionalized jejunal loop is then brought up in a retrocolic style and ready for anastomosis. Construction of Anastomosis For the needs of Roux-en-Y reconstruction, probably the most proximal loop of jejunum that can be brought to lie towards the deliberate web site of anastomosis with out pressure is chosen. The jejunum is transected, and a Roux limb of fifty to 70 cm is passed in a retrocolic trend by way of the avascular portion of the transverse mesocolon to the proper of the middle colic artery. The hepaticojejunostomy may be performed in an end-toside or side-to-side anastomosis (see Chapter 42). For an endto-side hepaticojejunstomy, the bile duct phase is transected, and an adjoining jejunotomy is customary at a safe distance from the mesenteric margin of the bowel approximately 2 cm from the staple line. The jejunotomy length ought to be shorter than the ductotomy, because the bowel is extra pliable than the duct. These sutures are tied and reduce brief except for the 2 corner sutures, which are secured with clamps. The previously positioned row of anterior sutures is then used to full the anastomosis. Each needle is handed by way of the jejunum, tied, and minimize short; the nook keep sutures are then reduce. When decompression is undertaken at the degree of the proximal hepatic duct, increased size may be achieved by extending the incision onto the left hepatic duct. An anterior row of full-thickness, single interrupted 4-0 or 5-0 absorbable sutures, handed from outside to inside, are retracted to allow publicity for placement of the posterior row. Full-thickness, single interrupted 4-0 or 5-0 absorbable sutures approximate the inferior fringe of the duct to the superior fringe of jejunum. Following placement, the posterior row of sutures is tied with knots on the within. Placement of a sponge circumferentially across the anastomosis allows an intraoperative take a look at to affirm absence of a giant bile leak. To perform this anastomosis, the anterior surface of the duct is uncovered and opened longitudinally for a distance of two. The biliary-enteric anastomosis can then be completed in an identical manner as described for side-to-side hepaticojejunostomy (see earlier). A single interrupted anterior (or right) row of sutures allows exposure for placement of the posterior (or left) row, approximating duct to jejunum, adopted by completion of the anterior row (Winslow et al, 2009). After mobilization of hepatic flexure of the colon, a beneficiant Kocher maneuver is carried out to allow enough mobility of the duodenum to allow construction of a tensionfree anastomosis. This produces incisions that are perpendicular to each other (unlike the parallel configuration used during hepaticojejunostomy). As with the hepaticojejunostomy, the duodenotomy is generally shorter in length than the ductotomy. The anastomosis is then constructed in a way that anastomoses the bile duct transversely to the longitudinally-oriented duodenotomy.