Emorivir
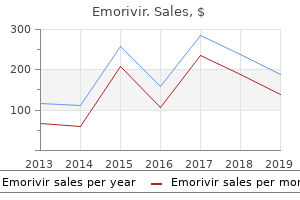
"Cheap emorivir 200 mg free shipping, highest hiv infection rates us".
By: H. Angar, M.B. B.CH. B.A.O., Ph.D.
Professor, Midwestern University Arizona College of Osteopathic Medicine
The cavernous sinuses (18) of the corpora cavernosa (15) are lined with endothelium and receive blood from the dorsal arteries (1 hiv infection rate zambia emorivir 200 mg generic, 14) and deep arteries (3) of the penis antiviral drugs for flu buy discount emorivir 200 mg line. The deep arteries (3) department in the corpora cavernosa (15) and kind the helicine arteries (6) hiv infection without penetration best 200mg emorivir, which empty instantly into the cavernous sinuses (18) how long after hiv infection symptoms cheap emorivir 200 mg overnight delivery. The cavernous sinuses (22) within the corpus spongiosum (21) obtain blood from the bulbourethral artery, a branch of the interior pudendal artery. Blood leaving the cavernous sinuses (18, 22) exits primarily via the superficial vein (12) and the deep dorsal vein (13). In the urethra (9) are invaginations referred to as urethral lacunae (of Morgagni) with mucous cells. Branched tubular urethral glands (of Littre) positioned under the epithelium open into these recesses. The lining of this portion of the urethra is a pseudostratified or stratified columnar epithelium (2). A skinny underlying lamina propria (5) merges with the encompassing connective tissue of the corpus spongiosum (9). Numerous outpockets or urethral lacunae (4) with mucous cells are located within the penile urethra (3) and are additionally linked with the mucous urethral glands (of Littre) (6, 7) within the connective tissue of the corpus spongiosum (9). The ducts from the urethral glands (6) open into the lumen of the penile urethra (3) throughout its size. The corpus spongiosum (9) consists of cavernous sinuses (1, 10) lined with endothelial cells and separated by connective tissue trabeculae (8) with clean muscle and collagen fibers. The excretory ducts of seminal vesicles be part of the vas deferens to form the ejaculatory ducts that enter the prostate gland and empty their secretions into the prostatic urethra. Their secretion enters the penile urethra, lubricates the penile urethra, and neutralizes the acidity of the urethra. This chemical is produced by the seminal vesicles that gives the power for sperm motility. Because mammary glands are part of the female reproductive system, their histologic structure and function are included on this chapter. During reproductive life, the human female reproductive organs exhibit cyclic month-to-month adjustments in construction and performance that characterize the menstrual cycle. The preliminary menstrual cycle is recognized as menarche, and when these cycles finally cease later in life, this phase represents the menopause. In addition, modifications within the uterine wall through the menstrual cycle are correlated with pituitary hormones and ovarian capabilities. These embrace the secretion of feminine intercourse hormones (estrogen and progesterone) for the event of feminine sexual characteristics, manufacturing of oocytes, offering suitable surroundings for the fertilization of the oocytes within the uterine (fallopian) tube, transportation of the creating embryo to the uterus and its implantation, vitamin and improvement of the fetus throughout being pregnant, and vitamin of the new child. In humans, a mature ovarian follicle ovulates and releases an immature egg known as the oocyte into the uterine tube roughly every 28 days. The transformation or maturation of the immature oocyte right into a mature egg or ovum occurs on the time of fertilization. At the moment of contact between the sperm and the cells across the oocyte, the corona radiata, an acrosomal response takes place that causes the release of the hydrolytic enzymes from the acrosome on sperm head. This motion dissolves the encircling cell layers around the oocyte, and the sperm penetrates the zona pellucida of the oocyte to fertilize it. One section of the ovary is connected to the broad ligament by a peritoneal fold known as the mesovarium and another part to the uterine wall by an ovarian ligament. The ovarian surface is covered by a single layer of cells known as the germinal epithelium that overlies the dense connective tissue tunica albuginea. Inferior to the tunica albuginea is the ovarian cortex that contains the ovarian follicles. Deep to the cortex is the vascularized, connective tissue core of the ovary, the medulla. During embryonic development, primordial germ cells migrate from the yolk sac and colonize the embryonic gonadal ridges. Here, the germ cells differentiate into oogonia via the method of mitosis and then enter the primary part of meiotic division without completing it. The germ cells turn into arrested on this state of development and at the moment are known as main oocytes. Primordial follicles are also formed throughout fetal life and encompass a main oocyte surrounded by a single layer of squamous follicular cells. Beginning at puberty and underneath the influence of pituitary hormones, some chosen primordial follicles develop and enlarge to turn into major, secondary, and large mature follicles, which can span the ovarian cortex and prolong into the medulla.
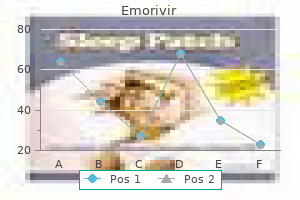
The separate tympanic duct (4) and vestibular duct (2) proceed in a spiral course to the apex of the cochlea hiv gi infection emorivir 200 mg, the place they impart through a gap known as the helicotrema (1) hiv infection by needle order emorivir 200mg on-line. The vestibular (Reissner) membrane (5) separates the vestibular duct (2) from the cochlear duct (scala media) (3) and varieties the roof of the cochlear duct (3) hiv infection experiences order emorivir mastercard. The vestibular membrane (5) attaches to the spiral ligament (11) in the outer bony wall of the cochlear canal (8) hiv infection rates nyc buy emorivir with amex. The sensory cells for sound detection are located in the organ of Corti (12), which rests on the basilar membrane (9) of the cochlear duct (3). A tectorial membrane (10) overlies the cells within the organ of Corti (12) (see additionally. The outer wall of the cochlear duct (9) is shaped by a vascular space referred to as the stria vascularis (15). The stratified epithelium masking the stria vascularis (15) accommodates a wealthy intraepithelial capillary network fashioned from the blood vessels that provide the connective tissue within the spiral ligament (17). The spiral ligament (17) accommodates collagen fibers, pigmented fibroblasts, and quite a few blood vessels. The roof of the cochlear duct (9) is formed by a thin vestibular (Reissner) membrane (6) that separates the cochlear duct (9) from the vestibular duct (scala vestibuli) (7). The vestibular membrane (6) extends from the spiral ligament (17) in the outer wall of the cochlear duct (9) positioned on the higher extent of the stria vascularis (15) to the thickened periosteum of the osseous 942 spiral lamina (2) close to the spiral limbus (1). The spiral limbus (1) is a thickened mass of periosteal connective tissue of the osseous spiral lamina (2) that extends into and varieties the floor of the cochlear duct (9). The spiral limbus (1) is covered by an epithelium (5) that appears columnar and is supported by a lateral extension of the osseous spiral lamina (2). The lateral extracellular extension of the spiral limbus epithelium (5) past the spiral limbus (1) forms the tectorial membrane (10) that overlies the inside spiral tunnel (8) and a portion of the organ of Corti (13). The basilar membrane (16) is a vascularized connective tissue that varieties the decrease wall of the cochlear duct (9). The organ of Corti (13) rests on the fibers of the basilar membrane (16) and consists of the sensory outer hair cells (11), supporting cells, related inside spiral tunnel (8), and an inner tunnel (12). The afferent fibers of the cochlear nerve (4) from the bipolar cells positioned within the spiral ganglion (3) course by way of the osseous spiral lamina (2) and synapse with outer hair cells (11) within the organ of Corti (13). A skinny, vestibular membrane (2) separates the cochlear duct (3) from the vestibular duct (scala vestibuli) (10). A thicker basilar membrane (7) separates the cochlear duct (3) from the tympanic duct (scala tympani) (14). The basilar membrane (7) extends from the connective tissue spiral ligament (6) to a thickened spiral limbus (11). The basilar membrane (7) helps the organ of Corti (8) with its sensory hair cells (5) and supportive cells. Extending from the spiral limbus (11) is the tectorial membrane (4) that covers a portion of the organ of Corti (8) and the outer hair cells (5). The sensory bipolar spiral ganglion cells (13) are located within the bony cochlea (1, 9). The afferent axons from the spiral ganglion cells (13) pass through the osseous spiral lamina (12) to the organ of Corti (8) the place their dendrites synapse with its hair cells (5). The micrograph focuses totally on the cochlear duct (2) and the cells and structures in the organ of Corti (14) situated on the basilar membrane (6). Visible within the organ of Corti (14) are the outer hair cells (12), the inside tunnel (13), and the outer tunnel 944 (5) that separates the cells. Superior to the outer hair cells (12) is the tectorial membrane (4), with the inside spiral tunnel (11) situated inferior to the tectorial membrane (4). The skinny vestibular membrane (8) separates the vestibular duct (scala vestibuli) (1) from the cochlear duct (2). Facing the cochlear duct (2) is the vascularized epithelium of stria vascularis (3) that overlies the connective tissue spiral ligament (7). The vestibular membrane (8) attaches to the spiral limbus (9) under which are found the axons of the cochlear nerve (10). Sound waves that enter the ear and move via the external auditory canal create mechanical vibrations within the tympanic membrane that activate the three bony ossicles (stapes, incus, and malleus) within the middle ear.
A larger primary follicle (4) with a primary oocyte (3) is surrounded by stratified cuboidal granulosa cells antiviral medication for genital warts cheap emorivir 200mg with amex. On the proper facet is a larger follicle with disorganized granulosa cells in the antrum and with pyknotic nuclei; this appears to be an atretic follicle (7) hiv infection flu like symptoms generic emorivir 200mg without prescription. Primordial follicles (14 antiviral quotes best 200mg emorivir, 17) are located within the cortex inferior to the tunica albuginea (16) hiv aids infection rates uk generic emorivir 200 mg amex, and each is surrounded by a single layer of squamous follicular cells (17). As the follicles develop larger, the follicular cells (17) of the primordial follicles (14, 17) change to cuboidal, or low 849 columnar, and the follicles now turn into major follicles (4, 11). The developing oocytes (4, 13) in the follicles also have a big eccentric nucleus (7, 13) with a nucleolus. In primary (growing) follicles (4, 11), the follicular cells proliferate by mitosis (3) and type layers of cuboidal cells known as the granulosa cells (8, 12) that encompass the first oocytes (4, 13). A single layer of the granulosa cells across the oocyte forms the corona radiata (5). Between the corona radiata (5) and the oocyte seems the noncellular glycoprotein layer known as the zona pellucida (6). The stromal cells that encompass the follicular cells now differentiate into the theca interna (9) layer positioned adjoining to the granulosa cells (8, 12). A thin basement membrane (not shown) separates the granulosa cells (8, 12) from the theca interna (9) cells. Many primordial, developing, or mature follicles exhibit degeneration, die, and are lost through atresia. A degenerating atretic follicle (1) is illustrated in the upper left nook of the illustration. Numerous blood vessels (2) encompass the growing follicles in the connective tissue of the cortex (15). The immature primordial follicles (2) include a major oocyte (3) surrounded by 850 a layer of easy squamous follicular cells (1, 7). As the primordial follicles (2) turn out to be main follicles (4), the layer of simple squamous follicular cells across the oocyte changes to a cuboidal layer. In a bigger primary follicle (8), the follicular cells have proliferated into a stratified layer known as granulosa cells (11). A distinguished layer of glycoprotein, the zona pellucida (10), develops between the granulosa cells (11) and the immature oocyte (9). The cells around the larger follicles manage into the internal hormonesecreting theca interna (12) and the outer connective tissue layer theca externa (13). The theca interna (12) and theca externa (13) are separated from the granulosa cells (11) by a skinny basement membrane (6). Surrounding the follicles in the cortex are the cells and fibers of the connective tissue (5). An area full of liquor folliculi is the antrum (3), displacing the first oocyte (10) on one aspect of the follicle. The main oocyte (10) rests on the cumulus oophorus (11), a mound of cells that additionally reveals separation because of accumulation of intercellular follicular fluid (12). The cells that encompass the oocyte form the corona radiata (5), although, on this picture, the separation between the oocyte and the corona radiata is due to the fixation course of. They are separated by a thin basement membrane (6) from the connective tissue which were altered to type the inner secretory epithelioid cells, the theca interna (2) layer and the outer connective tissue layer, the theca externa (8). On the proper aspect of the maturing follicle are the light-staining interstitial cells (7), which represent the remnants of the theca interna cells (2) that persist as particular person cells or as a gaggle of cells following follicular atresia. During the growth of the follicles, fluid accumulates between the granulosa cells across the oocyte, forming the antrum. This determine illustrates the cytoplasm and nucleus of a primary oocyte (3) of a mature follicle. A thickening of the granulosa cells (5) on one side of the follicle surrounds the first oocyte (3) and tasks into the antrum (4, 7) in kind a hillock (mound) referred to as the cumulus oophorus (8). The single layer of granulosa cells (5) adjacent to the first oocyte (3) types the corona radiata (1). Between the corona radiata (1) and the cytoplasm of the first oocyte (3) is the zona pellucida (2).
The pharmacist might compound capsules of a single medicinal agent or combination of brokers at the exact dosage prescribed for the individual patient antiviral zona zoster buy generic emorivir online. In the Conisnap Supro capsules hiv infection and aids difference buy emorivir with paypal, the upper capsule part extends thus far over the lower half that only the rounded fringe of the latter is visible symptoms of hiv reinfection discount emorivir 200mg. In addition to providing bulk antiviral liquid cheap emorivir 200mg on-line, these materials typically present cohesion to the powders, which is beneficial in the switch of the powder blend into capsule shells (2). Among the disintegrants used are pregelatinized starch, croscarmellose, and sodium starch glycolate. This is particularly important when a drug of low dosage is mixed with different medicine or nondrug fill (8). When essential, particle size may be lowered by milling to produce particles ranging from about 50 to 1,000 m. Depending on the supplies and tools used, micronization produces particles starting from about 1 to 20 m. In getting ready capsules on an industrial scale utilizing high-speed automated tools, the powder combine or granules must be free-flowing to allow steady passage of the capsule fill from the hopper via the encapsulating equipment and into the capsule shells. When magnesium stearate is used as the lubricant, the waterproofing traits of this water-insoluble material can retard penetration by the gastrointestinal fluids and delay drug dissolution and absorption. A surface-active agent, corresponding to sodium lauryl sulfate, is used to facilitate wetting by the gastrointestinal fluids to overcome the issue (9). Even if a waterinsoluble lubricant is used, after the gelatin capsule shell dissolves, gastrointestinal fluids should displace the air that surrounds the dry powder and penetrate the drug earlier than it can be dispersed and dissolved. This could also be accomplished to separate chemically incompatible agents or to add premeasured quantities of potent drug substances. Rather than weighing a potent drug, a pharmacist could select to insert a prefabricated pill of the specified power in every capsule. On an industrial scale, coated pellets designed for modifiedrelease drug supply are also generally placed in capsule shells. Gelatin capsules are unsuitable for aqueous liquids as a result of water softens gelatin and distorts the capsules, leading to leakage of the contents. Eutectic mixtures of medication, or mixtures of agents that will be inclined to liquefy when admixed, may be combined with a diluent or absorbent corresponding to magnesium carbonate, kaolin, or gentle magnesium oxide to separate the interacting agents and to take up any liquefied material that may form. When the standard dose of the drug is merely too large for a single capsule, two or more capsules may be required. In community apply, a person prescription might call for preparation of a few to a number of hundred capsules. To guarantee enough fill in the compounding of small numbers of capsules, the community pharmacist may calculate for the preparation of 1 or two more capsules than required to fill the prescription. The selection of the capsule size for a business product is finished during product growth. The alternative is set by necessities of the formulation, including the dose of the energetic ingredient and the density and compaction characteristics of the drug and different parts. Hard gelatin capsules are used to encapsulate about 65 mg to 1 g of powdered materials. Oftentimes, in the extemporaneous compounding of prescriptions, the most effective capsule dimension to use is set by trial. Place the powders in a graduated cylinder and obtain the volume occupied by the powders. Divide the quantity by the variety of capsules to be prepared and this offers the amount that might be occupied by the powder for each capsule. Then add additional diluent to the graduated cylinder containing the opposite powders to the mark indicated for the whole volume of powder required. The following examples demonstrate the drug and nondrug contents of some commercially obtainable capsules. The powder to be encapsulated is positioned on a sheet of clean paper or on a glass or porcelain plate. Using the spatula, the powder combine is fashioned right into a cake having a depth of roughly one-fourth to one-third the length of the capsule body. Then an empty capsule body is held between the thumb and forefinger and punched vertically into the powder cake repeatedly till filled.
Generic emorivir 200mg on line. HIV || AIDS - Part 2 : Testing Diagnosis Treatment in ENGLISH || Dr. ROOPAM JAIN.