Himplasia
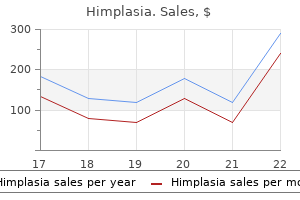
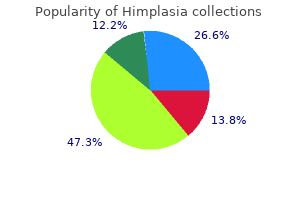
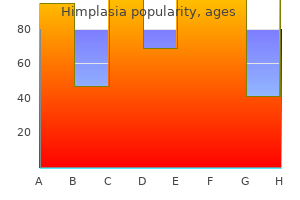
Himplasia dosages: 30 caps
Himplasia packs: 1 bottles, 2 bottles, 3 bottles, 4 bottles, 5 bottles, 6 bottles, 7 bottles, 8 bottles, 9 bottles, 10 bottles

30 caps himplasia discount overnight delivery
Beyond 12 months herbals scappoose oregon buy himplasia 30 caps mastercard, spontaneous restoration is often unlikely and intervention is indicated herbs paint and body himplasia 30 caps cheap online. In other circumstances, the affected person presents previous to tumor resection and should be endorsed concerning the want for facial nerve restore or grafting as nicely as static and dynamic procedures for reanimation. Occasionally, facial nerve division or resection is unplanned prior to oncologic surgery, but reconstruction turns into indicated intraoperatively because of sudden tumor involvement or inadvertent damage. If the facial nerve is divided within the temporal bone or intracranially, there may be a deficit in style as a end result of lack of chorda tympani perform, or hyperacusis due to loss of stapedius muscle function. During the examination, the affected person is requested to elevate the eyebrows, close the eyes, smile, pucker the lips, and show the decrease enamel to assess operate of every of the main facial nerve branches. A "snap check" is carried out to assess decrease lid tone, and the presence of epiphora is noted. Loss of the nasolabial crease, deviation of the philtrum, commissure despair, and deviation of the lips and nose towards the traditional side are signs of lack of facial muscular tone. The vector of mouth movement on the unaffected facet can also be recorded in preparation for either static suspension or dynamic smile reconstruction. Because the House-Brackmann1 grading system was designed to assess world facial nerve dysfunction quite than perform of individual branches, its usefulness in extracranial nerve harm is limited. Proximal transection of the nerve must be repaired, although the risk for synkinesis is higher. The remaining cranial nerves also wants to be examined, and deficits should be addressed appropriately. Electromyographic research can be helpful in predicting whether spontaneous restoration will occur in addition to in assessing whether viable motor endplates exist if a delayed nerve restore or cranial switch is being considered. Cable nerve grafts could be obtained by sacrifice of the nice auricular nerve, branches of the cervical plexus on the C3 and C4 ranges, or the sural nerve. Results of facial nerve repair following remedy for malignancy have been documented in only some studies. Facial Nerve Repair For nerve transections and resection of small segments, immediate direct nerve repair is indicated to present one of the best results by means of motor function. This may serve as the definitive procedure for facial reanimation, or it could act as a "babysitter" procedure to keep the facial muscle tissue from atrophying whereas awaiting axonal progress via cross-facial nerve graft(s). When the hypoglossal or masseteric nerve is used as a "babysitter," the nerve anastomosis is later taken down and replaced with a crossfacial nerve graft in ~ 6 to 12 months. Hypoglossal�facial nerve switch has been used to restore resting tone to the face. An end-to-end anastomosis has the drawback of inflicting unilateral tongue paralysis, with concomitant impairment of speech and swallowing operate. An end-to-side anastomosis, usually via an interposition graft, is a technique of decreasing the morbidity of this procedure. In end-to-side grafting, the epineurium is regionally removed and some (25 to 30%) of the hypoglossal nerve axons are transected so that they may grow into the distal facial nerve. Speech and swallowing morbidity in addition to synkinesis and mass motion with tongue movement have been proven to be greatly decreased utilizing an end-to-side approach. A process that has more recently turn out to be popular is the use of the masseteric branch of the trigeminal nerve for dynamic facial reanimation. The nerve usually takes an oblique course within the deep substance of the muscle, traveling from posterior superior to anterior inferior. Following the nerve distally permits sufficient 152 I Topics in Head and Neck Reconstruction of facial motion independent of neck and shoulder operate appears to be very troublesome. The phrenic nerve has additionally been used for facial reanimation however can cause marked contraction with coughing, laughing, and deep inspiration, and use of the phrenic nerve is contraindicated in patients with pulmonary illness. In our follow, the spinal accent and phrenic nerves are thought of last resorts. Cross-facial nerve grafting has the advantage of offering natural emotional activation with out retraining. In this procedure, a quantity of nerves on the traditional facet are sacrificed and related to a nerve graft, which is tunneled subcutaneously to the affected aspect of the face. Exposure of the contralateral regular nerve is normally carried out via a facelift incision and elevation of a skin flap; nerve branches are identified and mapped as they exit the anterior fringe of the parotid gland and travel toward the muscle tissue of facial features. The sural nerve is probably the most commonly used donor nerve for cross-facial nerve grafting owing to its length, availability, minimal donor-site morbidity, axonal density, and ease of harvest. Intraoperative mapping of the contralateral normal aspect is performed utilizing a nerve stimulator to determine redundant branches of the facial nerve that innervate the same teams of muscle tissue. Grafting of zygomatic and buccal nerve branches have been described most incessantly, again due to their comparatively extra valuable features and contribution to symmetry in repose. The course of the interposition nerve grafts is often throughout the higher lip or lower lip gentle tissue. Cross-facial nerve grafting has been described as either a one-stage or a two-stage process. Singlestage procedures reduce the number of surgeries required and patients may profit from quicker reinnervation. In a two-stage process, nerve graft(s) are sutured to the donor nerve department on the traditional aspect and tunneled to the affected facet and left there. Axonal progress is typically estimated to be ~ 1 mm per day, which supplies a tough information for the period of time needed earlier than the second stage is performed. For practical purposes, usually 6 to 12 months elapse earlier than the second stage is carried out. In the second stage, the distal finish of the nerve graft is exposed, the nerve is trimmed sharply to take away any neuroma, after which the nerve is sutured to the distal portion of the severed facial nerve on the paralyzed side. The nerve exits the skull base, passes between the condyle and coronoid strategy of the mandible, and lies on the deep surface of the masseter muscle. The masseteric nerve has a powerful motor impulse, which supplies robust muscular activation and a quick reinnervation time, normally inside 3 months. Unlike the hypoglossal nerve, the masseteric nerve is situated close to the route of the facial nerve, which normally implies that interpositional nerve grafting is unnecessary. Patients can learn to activate the facial muscle tissue by focusing on tongue or jaw contraction after hypoglossal or masseteric nerve transfer, respectively. With both procedure, synkinesis can occur, as can undesirable activation throughout mastication and speech. Cerebral cortical adaptation can happen after rehabilitation with masseteric nerve transfer, and emotional nerve activation has been reported. Additionally, management 10 benefit of two-stage procedures is that the severed facial nerve can be grafted to the masseteric or hypoglossal nerves as babysitter nerves whereas waiting for cross-facial axonal progress. The major drawback of cross-facial nerve grafting is that results are inconsistent, not only between surgeons, but in addition for single surgeons utilizing the identical method. Undesirable weakening of the traditional contralateral aspect is a possible risk that may be prevented by finding and using nondominant branches as donor nerves. Grafting of distal nerve branches, rather than of the proximal facial nerve trunk, minimizes the danger for synkinesis and facilitates spontaneous emotional facial motion without the need for retraining. Muscle tour is also normally much less sturdy than with masseteric or hypoglossal nerve switch. Because the regenerating axons should cross two suture strains and travel longer distances than ipsilateral donor nerves, reinnervation is gradual and usually solely partial.
Generic himplasia 30 caps free shipping
Plast Reconstr Surg 2009; 123:1220�1228 29 Supraclavicular Artery Island Flap Michael W herbs pool order 30 caps himplasia with visa. Chiu Introduction the supraclavicular flap has been successfully used for various difficult facial reconstruction instances herbs that heal himplasia 30 caps generic on line, offering acceptable results with out requiring microsurgical methods. In 1949, Kazanjian and Converse first described the fasciocutaneous flap and referred it because the acromial flap. Mathes and Vasconez performed the first anatomical examine of a supraclavicular artery-based flap in 1978, they usually named it the cervicohumeral flap. In 1983, Lamberty and Cormack named the supraclavicular artery-a vessel cephalad to the clavicular insertion of the trapezius muscle. It is a versatile flap consisting of skinny, pliable skin with a big arc of rotation and glorious color match for reconstruction of cervicofacial, scapular, and anterior chest wall defects. The location of the supply artery and the arc of rotation of the flap allow it to reliably attain most neck and decrease facial defects in addition to the tongue, the ground of the mouth, and hypopharyngeal defects. Although it can be used both as a regional (rotational, transpositional, interpolated) or a microvascular free flap, there are more attractive free flap choices when it comes to vascular pedicle length and vessel diameter. The supraclavicular artery on uncommon occasions can come up from the suprascapular artery. Anatomical studies and characterization of the supraclavicular artery have been performed in detail by a quantity of teams. Smaller cutaneous nerves have been additionally discovered posterior to the pedicle in a more distal location of the flap. Potential pitfalls and problems include distal tip ischemia, inadvertent transection of the pedicle during flap harvest, referred shoulder dysesthesia with stimulation of the skin paddle, and donor-site wound dehiscence or scarring. However, the scar is usually properly tolerated and delayed healing on the donor web site is uncommon. Anatomy of the supraclavicular artery island flap based mostly on fifty five cadaver dissections, suggests that the supraclavicular artery is current 80% of the time and has a diameter of 1. The arc of rotation for the supraclavicular flap, as a pedicled fascial flap or a tunneled island flap, has been reported as a lot as one hundred eighty levels. Consistent with other studies, the imply diameter of the supraclavicular artery was 1. Their research advised the pores and skin paddle is perfused beyond the deltoid muscle in 9 out of 10 cadaveric dissections. Sensory cervical nerves could be harvested with the supraclavicular flap and probably used to provide sensation to the reconstructed space. The senior author found that 20% of sufferers in his preliminary case series reported referred sensation to the shoulder in response to contact with the flap skin paddle. Branches of the supraclavicular nerves, from cervical roots C3 and C4, were discovered to emerge from the deep fascia at a separate location from the vascular pedicle. The nerve branches proximal to the pedicle, with one department exiting anterior to the flap and one other operating axially along the size of the flap. In this study, 9 out of ten flaps had major cutaneous nerves positioned 1 to 2 cm anterior to the pedicle, and one out of ten flaps had a significant cutane- Patient Positioning and Skin Markings During preoperative assessment, the course of the supraclavicular artery should be identified utilizing a handheld Doppler ultrasound in the workplace. The vessel is situated within the posterior triangle of the neck, whose boundaries are the sternocleidomastoid muscle, trapezius muscle, and the clavicle, and runs toward the acromion. On the day of surgical procedure, previous to the induction of common anesthesia, the pedicle location is confirmed once more. A suture may be fixated on the pivot level and the radius of rotation and pores and skin paddle length may be estimated and marked out with a surgical marker. An elliptical pores and skin paddle is then designed based on the defect and likewise consists of an extra 2 to 3 cm of skin medial to the pedicle origin. The widest a half of the elliptical pores and skin paddle ought to be 6 to 8 cm, relying on the skin laxity of the shoulder area, to enable major closure; the size can prolong up to three cm distal to the acromion. The neck, chest, and higher arm (circumferentially to elbow) are prepped and draped sterilely; the hands, forearm, and elbow are wrapped with a stocking and gauze, then the padded arm is tucked to the side. Once the flap dissection is accomplished lateral to the pedicle, the remaining medial pores and skin incisions are carried out to full the skin island paddle. Donor-Site Care the encompassing pores and skin of the donor website is widely undermined and can be closed primarily for skin paddles as much as 6 to 8 cm in width. If rigidity is extreme, a split-thickness skin graft could be performed and a negative-pressure wound dressing utilized. Tracheostomy ties and strain across the donor web site and vascular pedicle are to be averted, and dry dressings are used to prevent soilage from tracheostomy secretions. Operative Technique the pores and skin incision is carried down via the pores and skin and subcutaneous tissue by way of the fascia of the anterior deltoid muscle. As the flap is harvested more proximally, the underside of the flap is checked with a sterile handheld Doppler to verify vascular circulate. A vascular signal typically may be obtained all the way in which to the most lateral extent of the flap. Blunt dissection and bipolar cautery are used when the flap harvest is inside 2 to three cm of the pedicle origin to keep away from thermal damage to the vessel. The pedicle can also be visualized within the medial third of the flap by transillumination of the pores and skin. If multiple vessels are perfusing the flap, small vascular clamps can be utilized to occlude collateral vessels to confirm adequate pedicle blood circulate. Proximally, a 1 to 2 cm cuff of soft tissue/fat surrounding the pedicle is preserved to avoid harm to the source vessel. Electrocautery was used to elevate the flap distally, then bipolar cautery and blunt dissection were used to full the flap harvest near the vascular pedicle. At 12-month follow-up, the affected person was disease free, had a viable skin island, and had improved mouth opening. Women who wear strapless attire ought to be informed preoperatively about the donor-site scar. Flap thinning and revision are performed no sooner than 6 months after the conclusion of radiation. The fasciocutaneous supraclavicular artery island flap for releasing postburn mentosternal contractures. Plast Reconstr Surg 1997;99(7):1878�1884, discussion 1885�1886 Pallua N, Magnus Noah E. The tunneled supraclavicular island flap: an optimized method for head and neck reconstruction. Plast Reconstr Surg 2000;105(3):842� 851, dialogue 852�854 Di Benedetto G, Aquinati A, Pierangeli M, Scalise A, Bertani A. From the "charretera" to the supraclavicular fascial island flap: revisitation and further evolution of a controversial flap. Plast Reconstr Surg 2005;115(1):70�76 Abe M, Murakami G, Abe S, Sakakura Y, Yajima T. Supraclavicular artery in Japanese: an anatomical basis for the flap using a pedicle containing a cervical, nonperforating cutaneous branch of the superficial cervical artery. Reconstruction of neck scar contractures using supraclavicular flaps: retrospective examine of 30 circumstances.
Proven himplasia 30 caps
In 2003 the American Academy of Pediatrics issued a policy assertion indicating that ipecac syrup was not to be used routinely to treat poisonings at residence and that folks should discard any ipecac herbals on express himplasia 30 caps order fast delivery. If a fruitful emesis has occurred spontaneously shortly after ingestion rumi herbals chennai himplasia 30 caps order on line, further emesis is probably not needed. Ingestions of caustics, corrosives, ammonia, and bleach are definite contraindications to induced emesis. The speedy onset of coma or seizures or the potential to exaggerate the poisonous results of the poison might preclude additional the induction of emesis. Some examples embrace poisonings with opioids, clonidine, tricyclic antidepressants, hypoglycemic agents, nicotine, strychnine, -blocking agents, and calcium channel blockers. Debilitated, pregnant, and elderly patients may be further compromised by induction of emesis. Hospital Treatment Supportive and symptomatic care is the mainstay of remedy of a poisoned patient. Establishment of sufficient oxygenation and upkeep of adequate circulation are the very best priorities. Other parts of the acute supportive care plan embody the administration of seizures, arrhythmias, hypotension, acid-base stability, fluid standing, electrolyte steadiness, and hypoglycemia. Gastric Lavage Gastric lavage includes the location of an orogastric tube and washing out of the gastric contents through repetitive instillation and withdrawal of fluid. If the affected person is comatose or lacks a gag reflex, gastric lavage must be carried out only after intubation with a cuffed or well-fitting endotracheal tube. Relative contraindications for gastric lavage embrace ingestion of a corrosive or hydrocarbon agent. Complications of gastric lavage embody aspiration pneumonitis, laryngospasm, esophageal and gastric perforation and fluid and electrolyte imbalance. It is a highly purified, adsorbent form of carbon that forestalls gastrointestinal absorption of a drug by chemically binding (adsorbing) the drug to the charcoal floor. Activated charcoal is most effective when given throughout the first few hours after ingestion, ideally throughout the first hour. Activated charcoal is mixed with water to make a slurry, shaken vigorously, and administered orally or through a nasogastric tube. Activated charcoal has been promoted for use at house as a alternative for ipecac syrup, however some have contended that little evidence signifies activated charcoal can be used safely and properly on this setting. Activated charcoal is comparatively nontoxic, but two risks embrace (a) emesis following administration and (b) pulmonary aspiration of charcoal and gastric contents resulting in pneumonitis in patients with an unprotected airway or absent gag reflex. Infants, the elderly, and patients with impaired kidney perform should be given saline cathartics cautiously, if in any respect. These solutions also can be used to decontaminate the gastrointestinal tract of ingested toxins. It shortly causes gastrointestinal evacuation and is sustained till the rectal discharge is comparatively clear. Only 20% to 25% of patients complete a full routine of whole bowel irrigation based on poison center suggestions. This procedure may be indicated for sure sufferers in whom the ingestion occurred several hours prior to hospitalization and the drug nonetheless is suspected to be within the gastrointestinal tract, similar to drug smugglers who swallow condoms crammed with cocaine. Emesis, abdominal cramps, and intestinal bloating have been reported with whole-bowel irrigation. A medical coverage assertion by the American College of Emergency Physicians concludes that although no definitive advice can be made on the use of ipecac syrup, gastric lavage, cathartics, or whole-bowel irrigation, activated charcoal is advocated for most patients when appropriate. In many cases remedy solely with activated charcoal or observation and supportive care must be considered. Poison management facilities may be a source of guidance on the up to date application of gastric decontamination strategies for a selected patient. Enhanced Elimination Of the methods tried to improve the rate of excretion of poisons from the physique, solely diuresis, multiple-dose activated charcoal, and hemodialysis have demonstrated usefulness in select situations. These approaches should be thought-about only if the risks of the procedure are considerably outweighed by the expected advantages or if the recovery of the affected person is significantly doubtful and the tactic has been proven to be helpful. Diuresis Diuresis can be utilized for poisons excreted predominantly by the renal route; however, most medication and poisons are metabolized, and thus solely a great urine circulate (eg, 2-3 mL/kg/h) must be maintained for most patients. Ionized diuresis by altering urinary pH might increase excretion of certain chemical substances which would possibly be weak acids or bases by trapping ionized drug in the renal tubule and minimizing reabsorption. Complications of urinary alkalinization include alkalemia, hypokalemia, alkalotic tetany, and incapability to achieve target urinary pH values. This course of, termed charcoal intestinal dialysis or charcoal-enhanced intestinal exsorption, describes the attraction of drug molecules throughout the capillary bed of the gut by activated charcoal in the intestinal lumen and subsequent adsorption of the drug to the charcoal. Systemic clearance of several medication has been shown to be enhanced up to several-fold. The response to multiple-dose activated charcoal is biggest for drugs with the next characteristics: good affinity for adsorption by activated charcoal, low intrinsic clearance, adequate residence time in the body (long serum half-life), long distributive section, and low or nonrestrictive protein binding. A typical dosage schedule is 15 to 25 g of activated charcoal every 2 to 6 hours till serious symptoms abate or the serum focus of the toxin is below the toxic range. This procedure has been utilized in untimely and full-term infants in doses of 1 g/kg each 1 to four hours. Serious complications, such as pulmonary aspiration, occur in lower than 1% of patients. Dialysis must be considered when the length of signs is expected to be prolonged, regular pathways of excretion are compromised, medical deterioration is current, the drug is dialyzable (ie, cleared by dialysis hemofilters), and appropriate personnel and tools are available. Drugs which are dialyzable sometimes exhibit comparable physiochemical and pharmacokinetic properties that collectively render them amenable to extracorporeal clearance. For instance, medication exhibiting a low molecular mass (<1,000 daltons), low protein binding (<80%), and a small to modest volume of distribution (<1 L/kg) are usually dialyzable. Although hemodialysis can provide an efficient means of enhanced elimination, it could pose serious risks associated to anticoagulation, blood transfusions, lack of blood elements, fluid and electrolyte disturbances, and infection. Hemodialysis could also be lifesaving for methanol and ethylene glycol poisoning and effective for other poisons, such as lithium, salicylates, ethanol, and theophylline. Specific systemic antidotes can be found for many common poisonings (Table e9-9). Drugs used conventionally for non-poisoning situations may act as antidotes to reverse acute toxicity, similar to insulin-dextrose or glucagon for -adrenergic blocker or calcium channel antagonist overdose and octreotide for sulfonylureainduced hypoglycemia. There are a number of dosing schemes that involve single or multiple boluses followed by a continuous infusion, however none are properly studied. Lastly, the use of toxin-specific antibodies (eg, fragment antigen binding [Fab] antibody fragments for digoxin or North American crotaline snake venom) has provided a new approach to remedy of poisoning victims. Extrapolation of knowledge from human volunteer research to sufferers who overdose is troublesome because of potential or unknown variations in pharmacokinetics (eg, differing dissolution, gastric emptying, and absorption rates) seen with toxic versus therapeutic doses,17,18 differences in time to institute remedy within the emergency setting, and variations in absorption in fasted human volunteers compared with the complete abdomen of some sufferers who overdose. However, these studies present the most controlled and objective measures of the efficacy of a remedy.
Buy himplasia 30 caps lowest price
The neck is irrigated with an ample amount of normal saline and is returned to a impartial place herbals for high blood pressure himplasia 30 caps buy cheap on line. The radial forearm flap is sewn to the remaining tracheal wall on the recipient vessel facet first herbals india himplasia 30 caps best, before revascularization, using 3�0 polyglactin sutures. The small monitoring pores and skin flap, primarily based on a perforator vessel in the proximal forearm, is introduced outdoors the neck through the neck incision for flap monitoring functions and is removed at bedside earlier than discharge. A Dobhoff nasogastric feeding tube is placed for momentary feeding in the course of the acute postoperative interval. Follow-up imaging studies are performed for tumor surveillance and to assess the reconstructed trachea. Because of the absence of a larynx, the objective of tracheal reconstruction is to repair the tracheostoma or to extend the tracheostoma from the mediastinal trachea to the neck above the sternal notch with a gentle tissue flap. A second pores and skin paddle based on an independent perforator is used for tracheostoma reconstruction. When a total laryngectomy and whole esophagectomy with intensive tracheal resection are performed, Postoperative Care Meticulous perioperative care is given as a part of a combined staff effort. Bronchoscopy via the T-tube is performed day by day for three days to assess flap viability and airway patency and to clear secretions. Because many patients have unilateral vocal wire paralysis, a bedside swallowing take a look at is given to all patients by a speech pathologist before feeding is tried during recovery. Neck drains are eliminated as soon as drainage is lower than 30 mL in a 24-hr period for 2 consecutive days with no air leak. The monitoring skin flap exterior the neck is eliminated at the bedside 5 to 7 days after surgery. Bronchoscopy is performed earlier than discharge and at 6-month follow-up or as clinically indicated. The 5 Reconstruction of Tracheal Defects the remaining trachea above the carina is normally only three to 4 cm long. Therefore, double free flap reconstruction for the esophagus and trachea is indicated. The complete esophagectomy defect requires a supercharged jejunal flap to reach all the method in which to the base of the tongue. The second mesentery vessels are often used for supercharging in the neck to either the transverse cervical vessels or the internal mammary vessels. A small segment of jejunum primarily based on one or two terminal mesentery vessels is separated and later externalized for monitoring objective. The primary jejunal flap is then sewn to the base of the tongue and posterior pharynx. The second mesentery vessels are often used for supercharging within the neck either to the transverse cervical vessels or internal mammary vessels. The fourth mesentery vessels function the vascular pedicle for the pedicled portion of the flap. The jejunal flap is placed in a long plastic bag and pulled via the mediastinum to the neck. The distal end of the flap could be reliably extended past the anterior axillary fold for a width of 5 to 6 cm and size of 13 to 15 cm. Such an extended and narrow island flap continues to be well perfused and is suitable for tracheostoma and anterior neck reconstruction. A width of 5 to 6 cm can usually be closed primarily to keep away from donor-site deformity. These sufferers normally require the removal of the manubrium and unilateral clavicular head to get entry to the mediastinal trachea for tumor resection. Therefore, muscle flap coverage of the nice vessels is crucial to forestall catastrophic complications. If a radial forearm flap is planned, the pectoralis main muscle flaps can be utilized. The distal end of the flap can be reliably prolonged past the anterior axillary fold for a width of 5 to 6 cm and a size of 13 to 15 cm. They are based mostly on the internal mammary perforators in the second intercostal area which are usually the biggest. The concern regarding utilizing pores and skin for the tracheal lining stems from the likelihood that the shedding of keratin debris into the bronchial system could cause airway irritation and an infection. Long-term follow-up of our patients means that they tolerate skin lining properly, with no respiratory signs. It is likely that a small quantity of keratin shedding can be simply cleared by coughing. Our animal study showed that a Air Leak through the Anastomosis Air leakage is the most typical surgical complication after tracheal reconstruction and usually occurs throughout coughing. Most patients have their cricoid cartilage resected, and the flap is sewn to the thyroid cartilage. The thyroid cartilage is severely calcified in most sufferers, with a really thin mucosal lining. Healing between the pores and skin flap and calcified thyroid cartilage may be delayed, a supply of leakage. Small leaks produce minimal symptoms and are usually detected by subcutaneous emphysema or imaging research. A catheter placed percutaneously under computed tomographic steerage is ninety I Topics in Head and Neck Reconstruction adequate for managing minor leaks. The catheter can be connected to a PleuroVac in a manner much like the administration of pneumothorax. Coverage of the anastomosis with a muscle flap at initial surgical procedure may scale back the danger of air leak. Placement of a T-tube at the time of reconstruction can additionally be essential to forestall high airway strain throughout coughing so as to minimize air leakage. Resection for bronchogenic carcinoma involving the carina: longterm outcomes and impact of nodal status on outcome. Sleeve resection and prosthetic reconstruction of the pulmonary artery for lung most cancers. Intrathoracic tracheal reconstruction with a collagen-conjugated prosthesis: evaluation of the efficacy of omental wrapping. Experimental reconstruction of the canine trachea with a free revascularized small bowel graft. Tracheal reconstruction using a free jejunal flap with cartilage skeleton: experimental examine. Laryngoscope 2002;112(3):439�444 Delaere P, Vranckx J, Verleden G, De Leyn P, Van Raemdonck D; Leuven Tracheal Transplant Group. Otolaryngol Head Neck Surg 1989;100(2):119�125 Kunachak S, Kulapaditharom B, Vajaradul Y, Rochanawutanon M. Cryopreserved, irradiated tracheal homograft transplantation for laryngotracheal reconstruction in human beings.
30 caps himplasia discount free shipping
We sometimes begin with 2 to 4 mg diluted to 1 mg/mL herbals on express 30 caps himplasia generic with amex, primarily based on our own expertise herbals images himplasia 30 caps buy with visa. In the meantime, the surgical field should be gently irrigated with heat saline and covered with a heat towel to avoid vessel spasm. It may take 20 to 30 minutes for the flap to regain perfusion after such management. Once good venous outflow is obtained, the vein could be left open to drain out the thrombolytic brokers in the flap before re-anastomosing the veins to keep away from systemic effect of thrombolytic brokers. Hematoma Reasons for hematoma include basic oozing from the surgical bed, inadequate cautery or ligation of the vessels, and reopening of the vessels after hypertension or agitation. Hematoma within the head and neck area must be evacuated immediately in the working room as a end result of most, if not all, hematomas will get infected because of long exposure and contamination. In addition, hematoma can compress the flap pedicle, inflicting pedicle thrombosis, or it might be a sign of thrombosis of the vein on the anastomosis, causing blood to ooze from the flap. Thorough exploration of the surgical area must be carried out, and the flap vascular pedicle also needs to be explored for bleeding. After hematoma evacuation and correct hemostasis, the complete surgical field ought to be thoroughly irrigated with regular saline and possibly antibiotic-containing saline to minimize the danger of infection. Care should be taken not to irrigate the saline directly on the vascular pedicle, which may trigger spasm and thrombosis. Large hematomas within the donor web site should be explored, while small hematomas without active bleeding could be noticed. Such hematomas will usually liquefy after 7 to 10 days, and increased drainage of dark blood can be observed in donor-site drains. Wound Infection Neck wound an infection normally happens between 5 and 10 days after surgery, most commonly round 6 or 7 days. The infection rate is reported to be between 10% and 20% after a serious surgery and reconstruction. The main purpose for such a high wound infection fee is the prolonged contamination at the time of surgery. Any lifeless area, nonviable tissue, or hematoma could cause infection; due to this fact, they should be taken care of promptly. Including a small amount of flap muscle is usually a very effective approach to get rid of dead space and reduce infection. Several liters of regular saline or 186 I Topics in Head and Neck Reconstruction antibiotic resolution may be wanted to irrigate a big wound. Although many patients manifest with a fever, increased white blood cell rely, and erythema and swelling across the incision, medical manifestations could also be very refined in some sufferers, such because the elderly, diabetic, and immunocompromised. Once an early an infection is suspected, incision and drainage in the working room with enough exposure should be carried out, adopted by thorough d�bridement and irrigation. For early wound infections with out useless space, the neck incision can potentially be closed primarily over a drain or solely a small portion of the incision left open for dressing modifications after an intensive d�bridement. Pearls and Pitfalls � Meticulous postoperative care is crucial not only to patient restoration but also to prevent flap loss due to unsatisfactory fluid quantity status and issues with positioning, which may trigger pedicle or flap compression. Wound Dehiscence or Skin Graft Loss Small wound dehiscence either at the donor website or recipient website could be managed with dressing modifications to permit secondary healing. Surgical closure of the wound dehiscence within the head and neck area is unlikely to succeed. Partial skin graft loss at the donor site can also be managed with dressing changes. Leaks and Fistulas Leaks are outlined as radiographic leaks with no medical fistula, while a fistula is defined as a clinically evident fistulation between the oropharyngeal cavity and the skin pores and skin. Small leaks with out scientific infection or fistula could be observed conservatively and oral intake should be delayed. Small fistulas can additionally be observed conservatively, and they should heal spontaneously inside 2 to 4 weeks. Large leaks with fluid collection, useless house, or infection must be taken care of surgically. After d�bridement, a muscle flap, corresponding to a sternocleidomastoid muscle or pectoralis main muscle flap, can be utilized to obliterate the useless space, which also wants to be positioned over the flap dehiscence from the oral or pharyngeal mucosa. Attempt to close the dehiscence at this stage is normally unsuccessful and will cause extra tearing of the encompassing tissue. Timing of presentation of the first indicators of vascular compromise dictates the salvage consequence of free flap transfers. Analysis of 49 circumstances of flap compromise in 1310 free flaps for head and neck reconstruction. The impact of an implantable Doppler probe on the salvage of microvascular tissue transplants. Tissue pH monitoring in microsurgery: a preliminary evaluation of continuous tissue pH monitoring as an indicator of perfusion disturbances in microvascular free flaps. Monitoring buried free flaps: limitations of the implantable Doppler and use of color duplex sonography as a confirmatory test. Doppler ultrasound floor monitoring of both arterial and venous circulate in medical free tissue transfers. Implantable venous Doppler microvascular monitoring: laboratory investigation and clinical results. The combination of dying of osteoblasts, failure of osteoblasts to repopulate, and excessive proliferation of myofibroblasts ends in a reduction in bony matrix and its replacement with fibrous tissues. Finally, progressive fibrosis ends in mechanical destabilization and subsequent pathologic fracture. The dominant blood provide to the body of the mandible is the inferior alveolar artery, and radiation causes obliteration of this artery. The most vulnerable site of the mandibular body is the premolar, molar, and retromolar cortex, owing to the lack of muscular attachments and primary dependence on the inferior alveolar artery for its blood supply. There is mucosal disruption and dysfunction, salivary gland failure resulting in decreased manufacturing of salivary enzymes, xerostomia, parotid irritation, and fibrosis. Radiologic evaluation features a Panorex plain movie to consider the entire mandible for cortical erosion and fracture. Addressing these issues previous to radiation therapy, with extractions in a nonradiated area, is far preferable to postradiation dental extractions. Postradiation dental extractions have the next fee of complications from nonhealing sockets that enable uncovered alveolar bone to turn out to be desiccated and necrotic. The first step is to identify potential danger components in all patients present process radiation therapy. Maintaining sufficient oral hygiene, fluoride complement treatments, correctly fitting oral appliances, and frequent intraoral exams and follow-up visits with dental oncologists are the mainstays of preventative look after radiated sufferers. Thorough dental screen- 190 I Topics in Head and Neck Reconstruction Surgical Management Indications for Surgery 1. Reconstruction may be extraordinarily tough, and a careful operative plan is of paramount significance. Donorsite assessment normally contains fibula, anterolateral thigh flap, and radial forearm donor sites.
Himplasia 30 caps discount line
The most commonly accepted threat factors include obesity himalaya herbals products himplasia 30 caps purchase on-line, radiation herbals on deck review 30 caps himplasia purchase visa, infection and genetic factors. Cellulitis and infections have been reported to enhance the danger of gynecological and breast cancer-related lymphedema. For example, in a retrospective study of 67 patients treated for vulvar cancer, Gould et al. By providing evidence for genetic mutations as an necessary danger consider secondary lymphedema, these new discoveries problem the traditional perspective of secondary lymphedema being solely as a result of mechanical trauma. For example, a latest examine in breast most cancers patients found that solely 7% of sufferers who have been treated with radiation Summary Lymphedema is a disabling disorder that occurs as a consequence of primary abnormalities, harm, or infection to the lymphatic system. In developed countries, lymphedema occurs mostly as a consequence of most cancers treatment. Lymphedema in these circumstances develops 6 � Definition, Incidence and Pathophysiology of Lymphedema forty nine most incessantly in a delayed trend after surgery, usually months to years later. Diagnosis of lymphedema is predicated on history and bodily exam and is aided by physiologic/radiologic measures. Lymphedema staging is useful for classification of sufferers; nevertheless, the presently accepted strategies all rely on physical findings rather than physiologic changes within the lymphatic system. Recent research have supplied evidence that fibrosis and adjustments in adipose metabolism play an essential role within the pathology of lymphedema. These research provide a rationale for the recognized clinical danger elements for lymphedema including radiation, obesity, and recurrent infections, since these risk components enhance the danger of fibrosis and/or promote adipose deposition. Regardless, a better understanding of the pathology of lymphedema is important for development of novel methods designed to forestall or deal with this disabling illness. Development in selfreported arm-lymphedema in Danish women handled for early-stage breast cancer in 2005 and 2006 � A nationwide follow-up research. Prevalence of lymphedema in ladies with breast cancer 5 years after sentinel lymph node biopsy or axillary dissection: patient perceptions and precautionary behaviors. A up to date, population-based examine of lymphedema threat components in older girls with breast most cancers. Lymphedema past breast cancer: a scientific evaluate and meta-analysis of cancerrelated secondary lymphedema. The new era of the lymphatic system: now not secondary to the blood vascular system. The classification and diagnostic algorithm for major lymphatic dysplasia: an update from 2010 to embody molecular findings. Lymphedema in breast cancer survivors: incidence, degree, time course, remedy, and signs. The expertise of lower limb lymphedema for ladies after treatment for gynecologic cancer. Challenging the myth of exerciseinduced lymphedema following breast cancer: a collection of case reports. Effects of aerobic and resistance exercise in breast cancer patients receiving adjuvant chemotherapy: a multicenter randomized managed trial. Human lymphatic pumping measured in wholesome and lymphoedematous arms by lymphatic congestion lymphoscintigraphy. Improvement of higher extremity lymphedema after delayed breast reconstruction with an extended latissimus dorsi myocutaneous flap. Bioelectrical impedance evaluation: confirmed utility in lymphedema threat assessment and therapeutic monitoring. Prediction of therapy end result with bioimpedance measurements in breast cancer associated lymphedema patients. Breast and gynecologic cancerrelated extremity lymphedema: a evaluate of diagnostic modalities and administration choices. Pathological steps of cancerrelated lymphedema: histological adjustments in the amassing lymphatic vessels after lymphadenectomy. Characteristic indocyanine green lymphography findings in lower extremity lymphedema: the generation of a novel lymphedema severity staging system using dermal backflow patterns. Connexin forty seven mutations increase threat for secondary lymphedema following breast most cancers remedy. Expression of the fms-like tyrosine kinase 4 gene becomes restricted to lymphatic endothelium throughout growth. Signalling via vascular endothelial development issue receptor-3 is enough for lymphangiogenesis in transgenic mice. Vascular endothelial growth factor receptor-3 in lymphangiogenesis in wound therapeutic. Mutation in vascular endothelial growth factor-C, a ligand for vascular endothelial development issue receptor-3, is associated with autosomal dominant milroy-like main lymphedema. Autosomal recessive intestinal lymphangiectasia and lymphedema, with facial anomalies and psychological retardation. Th2 differentiation is important for soft tissue fibrosis and lymphatic dysfunction ensuing from lymphedema. Substitution of asparagine for serine-406 of the immunoglobulin mu heavy chain alters glycosylation at asparagine-402. Reduced adipose tissue lymphatic drainage of macromolecules in overweight topics: a possible link between obesity and native tissue inflammation Obesity impairs lymphatic fluid transport and dendritic cell migration to lymph nodes. Risk elements for lymphedema in a potential breast most cancers survivorship study: the Pathways Study. Risk factors for arm lymphedema following breast cancer prognosis in Black women and White girls. The epidemiology of arm and hand swelling in premenopausal breast most cancers survivors. An analysis of the etiological factors of lymphedema following radical mastectomy; an analysis of 1,007 circumstances. A randomized controlled trial of weight reduction as a therapy for breast cancer-related lymphedema. The indications for referral to conservative remedy are different from these for referral for surgical procedure. Knowing the extent to which the affected person is engaged with remedy helps focus the therapy approach and plan. Symptoms are necessary when setting targets for remedy, since what the affected person considers a successful consequence might differ from what is taken into account successful for the therapist, doctor, or healthcare system. Evidence within the literature helps the reliability of multiple approaches for the evaluation of the swollen limb. Assessment ought to begin with a radical historical past and physical examination to establish a correct analysis and care plan. Lymphedema is a persistent situation for which a remedy has not yet been identified; nevertheless, when identified early, intervention may reverse or reduce the situation to the pre-emergent state or reduce its debilitating effects.
30 caps himplasia generic free shipping
These reactions generally inactivate the pharmacologic exercise of the drug and may make it extra susceptible to herbals in hindi buy himplasia 30 caps cheap elimination by the kidney herbs los gatos cheap 30 caps himplasia otc. The kidney can excrete drugs by glomerular filtration or by such active processes as proximal tubular secretion. Drugs also may be eliminated through bile produced by the liver or air expired by the lungs. Linear Pharmacokinetics Most drugs comply with linear pharmacokinetics; serum drug concentrations change proportionally with long-term every day dosing. If the drug is given at intermittent dosage intervals, such as 250 mg every 6 hours, steady state is achieved when the serum-concentration-versus-time curves for every dosage interval are superimposable. Bioavailability and Bioequivalence When medication are administered extravascularly, drug molecules have to be launched from the dosage type (dissolution) and pass by way of several biologic obstacles earlier than reaching the vascular system (absorption). P-glycoprotein (P-gp) is the first transport protein that interferes with drug absorption by this mechanism. Special strategies are needed to determine the fraction of drug absorbed orally for medicine with excessive liver extraction ratios or substantial gut wall metabolism. When this happens, the serum-concentration-versus-time curves for the two dosage types must be superimposable and equivalent. Bioequivalence research have become very important as expensive medication turn out to be available in less costly generic kind. If the drug is administered as particular person doses (D) at a given dosage interval, the average Css over the dosage interval is given by the equation4 the place F is the fraction of dose absorbed into the systemic vascular system. Physiologically, clearance is determined by (a) blood circulate (Q) to the organ that metabolizes (liver) or eliminates (kidney) the drug and (b) the efficiency of the organ in extracting the drug from the bloodstream. Clearance adjustments happen in patients when the blood circulate to extracting organs changes or when the extraction ratio adjustments. Extraction ratios can improve when enzyme inducers increase the quantity of drug-metabolizing enzyme. Extraction ratios could lower if enzyme inhibitors inhibit drug-metabolizing enzymes or necrosis causes lack of parenchyma. In this case, clearance of the drug is the identical as blood circulate to the organ; such medicine are referred to as high-clearance medication and have massive extraction ratios. Propranolol, verapamil, morphine, and lidocaine are examples of high-clearance medication. High-clearance drugs corresponding to these usually exhibit excessive first-pass results when administered orally. In this case, clearance of the drug is equal to the product of the fraction unbound within the blood and the intrinsic capacity of the organ to clear unbound drug from the blood; such medicine are known as low-clearance drugs and have small extraction ratios. Warfarin, theophylline, diazepam, and phenobarbital are examples of low-clearance medication. As mentioned previously, the focus of unbound drug in the blood is probably more necessary pharmacologically than the total (bound plus unbound) focus. The unbound drug within the blood is in equilibrium with the unbound drug within the tissues and displays the concentration of drug at its website of motion. Therefore, the pharmacologic effect of a drug is assumed to be a perform of the focus of unbound drug in the blood. The unbound steady-state focus (Css,u) could be calculated by multiplying Css and fb: Css,u = Css fb. Because laboratories often measure only whole concentrations (concentrations of unbound drug are troublesome to determine), the interaction is hard to detect. For example, a low-clearance drug is administered to a patient until steady-state is achieved: Suppose that one other drug is administered to the patient that displaces the first drug from plasmaprotein-binding websites and doubles fb (fb now equals 2fb). The potential for error in this scenario is that clinicians might improve the dose of a low-clearance drug after a protein-binding displacement interplay because Css decreased. Low albumin concentrations (as in trauma or pregnant patients), high concentrations of endogenous plasma protein-binding displacers (as with excessive concentrations of bilirubin), or plasma protein-binding drug interactions (as with concomitant therapy with valproic acid) can lead to subtherapeutic whole phenytoin concentrations. Despite this truth, unbound phenytoin concentrations normally are throughout the therapeutic vary, and infrequently the patient is responding appropriately to treatment. Thus, in these conditions, unbound somewhat than whole phenytoin serum concentrations should be monitored and used to information future therapeutic decisions. Clearances for Different Routes of Elimination and Metabolic Pathways Clearances for particular person organs could be computed if the excretion the organ produces can be obtained. For example, renal clearance can be calculated if urine is collected during a pharmacokinetic experiment. Subsequent urine production is collected till the last serum focus (Clast) is obtained. This computation is especially helpful in drug-interaction research to decide which metabolic pathway is stimulated or inhibited. As ordinary, steady-state circumstances are achieved in three to 5 half-lives for the drug. The numeric worth for the volume of distribution is determined by the physiologic volume of blood and tissues and how the drug binds in blood and tissues:8 where Vb and Vt are the volumes of blood and tissues, respectively, and fb and ft are the fractions of unbound drug in blood and tissues, respectively. Half-Life Half-life (t1/2) is the time required for serum concentrations to decrease by one-half after absorption and distribution are full. Half-life is important as a outcome of it determines the time required to attain steady state and the dosage interval. It takes approximately three to five half-lives to reach steady-state concentrations throughout continuous dosing. In three half-lives, serum concentrations are at ~90% of their final steady-state values. For this purpose, many clinicians consider concentrations obtained after three half-lives to be Css. For example, it may be fascinating to preserve maximum steady-state concentrations at 20 mg/L and minimal steady-state concentrations at 10 mg/L. In this case, it would be essential to administer the drug each half-life as a outcome of the minimum fascinating concentration is one-half the utmost desirable focus. The elimination fee fixed (k) is expounded to the half-life by the following equation: k = zero. Both the half-life and elimination rate fixed describe how shortly serum concentrations decrease within the serum or blood. When this happens, the maximum fee of metabolism (Vmax) for the drug is approached. Most drugs eradicated by the liver are metabolized by enzymes but nonetheless appear to observe linear kinetics. The reason for this disparity is that the therapeutic vary for many drugs is well under the Km of the enzyme system that metabolizes the agent. When a dosage increase takes place, fb increases as a result of nearly all plasma protein-binding websites are occupied, and no binding websites can be found. Valproic acid9 and disopyramide10 both comply with saturable protein-binding pharmacokinetics. Autoinduction For some medicine, clearance increases as the dose or focus of the drug will increase. In this example, rising the drug dose or concentration increases the flexibility of the enzyme system to get rid of the compound and to clear the drug from the physique.
30 caps himplasia purchase with amex
Care should be taken to protect a few of the muscle/tendon attachment to the iliac crest to reduce useful disturbance herbals baikal himplasia 30 caps buy on-line. The lateral femoral cutaneous nerve and the ilioinguinal nerve should be recognized and preserved herbals vitamins buy himplasia 30 caps on-line. Using an oscillating noticed, the outer cortex of the iliac crest is reduce, followed by the internal cortex via the already divided iliacus muscle. Iliac Crest Flap 295 Modification of the Iliac Crest Flap�The Inner Cortex Iliac Crest Flap Because a full-thickness iliac crest harvest creates a disruption of the stomach wall muscle and thigh muscle attachment, the disruption might result in belly hernia formation and gait disturbance. To minimize these problems, the internal cortex could be harvested together with the superior rim of the iliac crest without detaching the thigh muscular tissues. After the decrease lateral pores and skin incision is made, the periosteum of the outer rim of the iliac crest is stripped down for just one cm without detaching the thigh muscle and tendon attachments. The bone is then cut up between the inner and outer cortices with a large periosteal elevator. The 1 cm fullthickness rim of the iliac crest provides additional energy to the bone flap. Deep Circumflex Iliac Artery Perforator Flap One of the primary disadvantages of the traditional iliac crest flap is the obligatory inclusion of the full-thickness abdominal wall musculature if the pores and skin paddle is required. The ensuing gentle tissue bulk is normally too large to be positioned intraorally and will obstruct tongue motility and intrude with oral function. With a tentative pores and skin paddle design centered on the perforators, the superior border of the pores and skin paddle is incised to lengthen medially above the inguinal ligament. Osteotomy is then performed with an oscillating saw 2 cm beneath the vascular pedicle. The external oblique fascia is then incised across the perforators, and intramuscular dissection is carried out to trace the perforator back to its major pedicle. There are, nonetheless, several perforators in the region that will come up from different arteries, such because the intercostal, lumbar, and iliolumbar arteries. The remainder of flap harvesting is similar to the traditional or internal cortex iliac flap. Donor-Site Care With the traditional iliac crest flap, removing of the wing of the ilium creates a disruption of the lateral stomach wall and the thigh muscle attachments. It is important to reattach the transversus muscle to the iliacus or the remaining iliac bone. It could additionally be helpful to drill several holes in the minimize edge of the ilium to reattach the transversus muscle. With the internal cortex flap, the belly muscle and fascia are sewn to the fascia of the thigh muscle attachments and the periosteum. Pearls and Pitfalls � Dissection of the skin paddle perforator quite than together with a cuff of abdominal wall muscle can significantly lower the bulkiness of the soft tissue component of the osteocutaneous iliac crest free flap. Because of the thinness of the performing capacity to incorporate a quantity of pores and skin muscle and the an iliac crest free flap, as publicity can the latissimus dorsi musculocutaneous flap paddles,be extraordinarily challenging. Superiority of the deep circumflex iliac vessels as the provision at no cost groin flaps. Plast Reconstr Surg 1997;100(7):1703�1709 Kimata Y, Uchiyama K, Sakuraba M, et al. Deep circumflex iliac perforator flap with iliac crest for mandibular reconstruction. The anatomical basis of the deep circumflex iliac artery perforator flap with iliac crest. A compound flap could be elevated with a segment of latissimus dorsi muscle as one component, and serratus anterior muscle, dorsal thoracic fascia, scapular bone, and/ or scapular or parascapular pores and skin flap. The multiplicity of perforators derived from descending and transverse branches of the thoracodorsal artery additionally present a separate twin paddle design for advanced reconstructions. Improper perforator choice with respect to perforator dimension, quantity, or location within the flap might trigger suboptimal perfusion, leading to partial or tip necrosis. The crowded surgical area attributable to the proximity of the donor website to the pinnacle and neck region makes a two-team method tough. When the skin is de-epithelialized, a dermo-adiposal paddle can be utilized to augment the delicate tissue contour of the facial area, corresponding to in progressive hemifacial atrophy. In spite of the appreciable measurement of the flap, the donor web site was closed primarily and an acceptable linear scar was left. Latissimus Dorsi Flap/Thoracodorsal Artery Perforator Flap the principle pedicle of the latissimus dorsi muscle, the thoracodorsal artery and vein, derive from the subscapular vessels, which are branches of the third segment of the axillary artery and vein. During their course in a cephalocaudal direction, the thoracodorsal vessels give off an angular branch to the tip of the scapula and branches to the subscapularis, teres major, and serratus anterior muscular tissues. The thoracodorsal artery and vein enter the deep surface of the latissimus dorsi muscle at the neurovascular hilus, the place the pedicle bifurcates right into a descending (lateral) branch and a transverse (medial) branch. The descending department courses parallel to the lateral border of the muscle at a variable distance from it. The transverse branch runs equally parallel to the medial (upper) muscle border. In less than 10% of cases, the thoracodorsal vessels divide into three or 4 main intramuscular branches. The thoracodorsal nerve, which comes from the posterior twine of the brachial plexus, supplies motor innervation to the latissimus dorsi muscle and runs with the thoracodorsal vessel to a neurovascular hilus. The nerve then divides into intramuscular branches in parallel with the vascular branching sample. On the entire, two to seven thoracodorsal artery perforators originate either from the descending (lateral) department or the transverse (medial) department of the thoracodorsal artery. More distally, extra perforators from the identical intramuscular branch could be found. The transverse branch of the thoracodorsal artery also supplies reliable perforators, and sometimes the largest perforator comes from this branch. The perforators located anterior to the free lateral border of the latissimus dorsi muscle derive from completely different supply vessels. In the proximal area, a perforator from a direct cutaneous department of the thoracodorsal artery can be found in up to 60% of sufferers, but the dimension and quality of this perforator are inferior to those of true musculocutaneous perforators. Perforators can also arise from the serratus anterior department of the thoracodorsal artery and from the lateral intercostal artery. In uncommon circumstances, these perforators course by way of the lateral portion 299 Anatomy the latissimus dorsi muscle acts as an extender, adductor, and medial (internal) rotator of the humerus. The aponeurotic origin extends from the seventh thoracic vertebra to the center outer rim of the iliac crest, and the muscle spirals across the tendon of the teres major muscle to insert onto the medial lip of the intertubercular groove of the humerus. Frequently, the nerve branches hitchhike with perforators to enter the subcutaneous tissue. However, mapping of thoracodorsal artery perforators with instruments like acoustic handheld Doppler, color Doppler sonography, and computed tomographic angiography could be requested preoperatively.