Arava
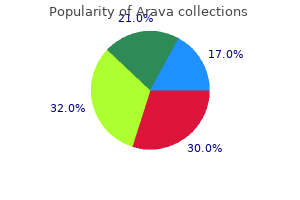
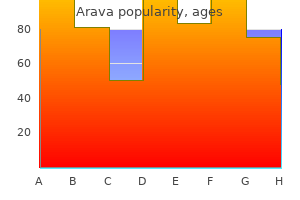
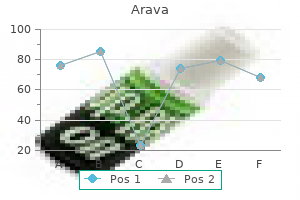
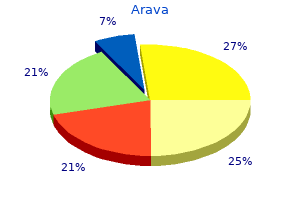
Arava dosages: 20 mg, 10 mg
Arava packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills

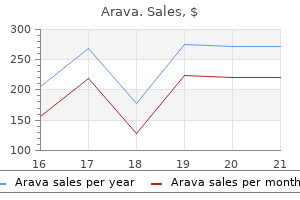
10 mg arava mastercard
Enter and synapse instantly with a postsynaptic neuron of the paravertebral ganglion at that level medicine chest order arava 10 mg with amex. Pass through the sympathetic trunk with out synapsing medicine side effects purchase arava 10 mg fast delivery, persevering with through an abdominopelvic splanchnic nerve (a department of the trunk involved in innervating abdominopelvic viscera) to reach the prevertebral ganglia. Presynaptic sympathetic fibers that provide autonomic innervation within the head, neck, physique wall, limbs, and thoracic cavity follow one of the first three courses, synapsing inside the paravertebral ganglia. Presynaptic sympathetic fibers innervating viscera within the abdominopelvic cavity follow the fourth course. Postsynaptic sympathetic fibers greatly outnumber the presynaptic fibers; every presynaptic sympathetic fiber synapses with 30 or extra postsynaptic fibers. By this implies, they enter all branches of all 31 pairs of spinal nerves, including the posterior rami. The postsynaptic sympathetic fibers stimulate contraction of the blood vessels (vasomotion) and arrector muscles associated with hairs (pilomotion, leading to "goose bumps"), and to cause sweating (sudomotion). Postsynaptic sympathetic fibers that perform these features within the head (plus innervation of the dilator muscle of the iris-dilator pupillae) all have their cell bodies in the superior cervical ganglion at the superior finish of the sympathetic trunk. They cross from the ganglion by the use of a cephalic arterial ramus (branch) to kind peri-arterial plexuses of nerves, which follow the branches of the carotid arteries, or they might cross directly to nearby cranial nerves, to reach their destination in the head (Maklad et al. Splanchnic nerves convey visceral efferent (autonomic) and afferent fibers to and from the viscera of the physique cavities. Postsynaptic sympathetic fibers destined for the viscera of the thoracic cavity. The presynaptic sympathetic fibers concerned in the innervation of viscera of the abdominopelvic cavity. All presynaptic sympathetic fibers of the abdominopelvic splanchnic nerves, besides those concerned in innervating the suprarenal (adrenal) glands, synapse in prevertebral ganglia. The postsynaptic fibers from the prevertebral ganglia form periarterial plexuses, which comply with branches of the belly aorta to attain their destination. The secretory cells of the medulla are postsynaptic sympathetic neurons that lack axons or dendrites. Consequently, the suprarenal medulla is provided instantly by presynaptic sympathetic neurons. The neurotransmitters produced by medullary cells are launched into the bloodstream to produce a widespread sympathetic response. The suprarenal medullary cells perform as a particular type of postsynaptic neuron that, instead of releasing their neurotransmitter substance onto the cells of a selected effector organ, release it into the bloodstream to flow into throughout the physique, producing a widespread sympathetic response. As described earlier, postsynaptic sympathetic fibers are elements of virtually all branches of all spinal nerves. Thus, the sympathetic nervous system reaches virtually all components of the body, with the rare exception of such avascular tissues as cartilage and nails. Because the two sets of sympathetic ganglia (para- and prevertebral) are centrally positioned within the body and are near the midline (hence relatively close to the spinal cord), on this division, the presynaptic fibers are relatively quick, whereas the postsynaptic fibers are comparatively lengthy, having to prolong to all components of the body. Not surprisingly, the cranial outflow provides parasympathetic innervation of the top, and the sacral outflow offers the parasympathetic innervation of the pelvic viscera. Regardless of the intensive influence of its cranial outflow, the parasympathetic system is much more restricted than the sympathetic system in its distribution. The parasympathetic system distributes only to the head, visceral cavities of the trunk, and erectile tissues of the external genitalia. Elsewhere, presynaptic parasympathetic fibers synapse with postsynaptic cell our bodies, which 226 occur singly in or on the wall of the target organ (intrinsic or enteric ganglia). This local activity is simply modulated by the enter from the extrinsic parasympathetic and sympathetic fibers. More detailed information about the enteric nervous system is offered in Chapter 5, Abdomen. In common, the sympathetic system is a catabolic (energy-expending) system that enables the body to deal with stresses, similar to when getting ready the body for the fight-or-flight response. The parasympathetic system is primarily a homeostatic or anabolic (energyconserving) system, promoting the quiet and orderly processes of the physique, such 227 as those who enable the body to feed and assimilate. Sympathetic fibers, by comparability, are distributed to all vascularized portions of the body. Blood vessels throughout the physique are tonically innervated by sympathetic nerves, sustaining a resting state of reasonable vasoconstriction. In most vascular beds, a rise in sympathetic signals causes increased vasoconstriction, and a lower within the price of sympathetic signals allows vasodilation. In the coronary vessels, the vessels of skeletal muscular tissues, and the external genitalia, sympathetic stimulation leads to vasodilation (Wilson-Pauwels et al. Visceral reflexes regulate blood stress and chemistry by altering such functions as coronary heart and respiratory charges and vascular resistance. However, sufficient stimulation, such as the next, could elicit visceral pain: Sudden distension. Pathological conditions (especially ischemia) that lower the conventional thresholds of stimulation. Normal exercise usually produces no sensation, but it may achieve this when the blood supply is inadequate (ischemia). Most visceral reflex (unconscious) sensation 229 and some pain travel in visceral afferent fibers that accompany the parasympathetic fibers retrograde (backward). Most visceral ache impulses (from the center and most organs of the peritoneal cavity) travel centrally along visceral afferent fibers accompanying sympathetic fibers. It is an important a half of clinical anatomy and is the anatomic basis of radiology, the department of medical science coping with the utilization of radiant energy within the diagnosis and therapy of illness. Being capable of determine normal constructions on radiographs (X-rays) makes it simpler to acknowledge the 231 changes caused by illness and harm. Familiarity with medical imaging techniques generally used in scientific settings permits one to recognize congenital anomalies, tumors, and fractures. The mostly used medical imaging methods are as follows: Conventional radiography (X-ray images). Medical imaging techniques permit the remark of anatomical structures in living folks and the examine of their movements in regular and irregular activities. Consequently, a dense tissue or organ produces a considerably clear area on the X-ray movie or brilliant area on a monitor as a end result of fewer X-rays attain the movie or detector. A dense substance is radiopaque, whereas a substance of much less density is radiolucent. This image demonstrates bone densities (light) of skeletal buildings, air densities (dark) of lungs and trachea, and soft tissue densities (intermediate) of the nice vessels and coronary heart and domes of the diaphragm. Note that the right dome of the diaphragm is higher, above the liver, and the left dome is decrease, inferior to the apex of the center. Portions of 234 the beam of X-rays traversing the physique turn out to be attenuated to various levels based mostly on tissue thickness and density. The beam is diminished by constructions that absorb or reflect it, inflicting less response on the movie or by the detector compared with areas that enable the beam to cross comparatively uninterrupted. Many of the same ideas that apply to making a shadow apply to standard radiography.
Cheap 10 mg arava visa
The 537 pulsations of the brachial artery help transfer the blood through this venous community medicine 48 12 arava 10 mg order. Not uncommonly medicine man 1992 order arava 20 mg amex, the deep veins be a part of to type one brachial vein during a part of their course. Their origins from the brachial plexus, courses within the higher limb, and the buildings innervated by them are summarized in Table three. After crossing the anterior side of the elbow, it continues to supply the pores and skin of the lateral facet of the forearm. The branch of the radial nerve to the lateral head of the triceps arises inside the radial groove. Anterior to the lateral epicondyle, the radial nerve divides into deep and superficial branches. The deep branch of the radial nerve is completely muscular and articular in its distribution. The superficial branch of the radial nerve is entirely cutaneous in its distribution, supplying sensation to the dorsum of the hand and fingers. The median nerve has no branches in the axilla or arm, but it does supply articular branches to the elbow joint. Posterior to the medial epicondyle, where the ulnar nerve is referred to in lay phrases as the "humorous bone. Like the median nerve, the ulnar nerve has no branches within the arm, however it additionally provides articular branches to the elbow joint. Medially, the mass of flexor muscles of the forearm arising from the common flexor attachment on the medial epicondyle; most particularly, the pronator teres. Laterally, the mass of extensor muscle tissue of the forearm arising from the lateral epicondyle and supra-epicondylar ridge; most particularly, the brachioradialis. The floor of the cubital fossa is formed by the brachialis and supinator muscle tissue of the arm and forearm, respectively. Radial nerve, deep between the muscular tissues forming the lateral boundary of the fossa (the brachioradialis, in particular) and the brachialis, dividing into its superficial and deep branches. Surface Anatomy of Arm and Cubital Fossa the borders of the deltoid are seen when the arm is abducted towards resistance. The long, lateral, and medial heads of the triceps brachii type bulges on the posterior aspect of the arm and are identifiable when the forearm is prolonged from the flexed position in opposition to resistance. It is separated from the skin by only the olecranon bursa, which accounts for the mobility of the overlying skin. The triceps tendon is definitely felt because it descends along the posterior facet of the arm to the olecranon. The fingers may be pressed inward on all sides of the tendon, the place the elbow joint is superficial. The biceps brachii tendon may be palpated within the cubital fossa, immediately lateral to the midline, especially when the elbow is flexed in opposition to resistance. The proximal part of the bicipital aponeurosis may be palpated where it passes obliquely over the brachial artery and median nerve. The cephalic vein runs superiorly in the lateral bicipital groove, and the basilic vein ascends within the medial bicipital groove. No part of the shaft of the humerus is subcutaneous; however, it can be palpated with varying distinctness through the muscle tissue surrounding it, particularly in many aged people. The head of the humerus is surrounded by muscular tissues on all sides, except inferiorly; thus, it can be palpated by pushing the fingers well up into the axilla. The humeral head could be palpated when the arm is moved while the inferior angle of the scapula is held in place. The brachial artery may be felt pulsating deep to the medial border of the biceps. The medial and lateral epicondyles of the humerus are subcutaneous and may be easily palpated at the medial and lateral features of the elbow. In the cubital fossa, the cephalic and basilic veins within the subcutaneous tissue are clearly seen when a tourniquet is applied to the arm, as is the median cubital vein. If the thumb is pressed into the cubital fossa, the muscular plenty of the long flexors of the forearm will be felt forming the medial border, the pronator teres most directly. The lateral group of forearm extensors (a soft mass that might be grasped separately), the brachioradialis (most medial) and the lengthy and short extensors of the wrist, can be grasped between the fossa and the lateral epicondyle. The anterior compartment incorporates three flexor muscle tissue provided by the musculocutaneous nerve. The posterior compartment accommodates a three-headed extensor muscle, the triceps, which is supplied by the radial nerve. Cubital fossa: the triangular cubital fossa is certain by a line connecting the medial and lateral epicondyles of the humerus, and the pronator teres and brachioradialis muscle tissue arising, respectively, from the epicondyles. In addition to firmly tying the forearm bones together while permitting pronation and supination, the interosseous membrane supplies the proximal attachment for some deep forearm muscle tissue. The head of the ulna is on the distal finish of the forearm, whereas the head of the radius is at its proximal finish. The position of forearm movement, occurring at the elbow and radio-ulnar joints, is to help the shoulder within the application of drive and in controlling the position of the hand in house. Dissection exhibiting the superficial muscle tissue of the forearm and the palmar aponeurosis. Compartments of Forearm As in the arm, the muscles of comparable purpose and innervation are grouped inside the identical fascial compartments within the forearm. Although the proximal boundary of the forearm per se is defined by the joint aircraft of the elbow, functionally the forearm contains the distal humerus. Their lengthy, slender tendons lengthen distally to the operative site, like long ropes reaching to distant pulleys. Furthermore, as a result of the structures on which the muscles and tendons act (wrist and fingers) have an extensive range of motion, a long range of contraction is needed, requiring that the muscular tissues have long contractile parts in addition to a long tendon(s). To present the required attachment websites for the flexors and extensors of the wrist and fingers, medial and lateral extensions (epicondyles and supra-epicondylar ridges) have developed from the distal humerus. At the extent of the cubital fossa, the flexors and extensor of the elbow occupy the anterior and posterior elements of the humerus. Lateral and medial extensions (epicondyles and supra-epicondylar ridges) of the humerus provide proximal attachment (origin) for the forearm flexors and extensors. Consequently, within the proximal forearm, the "anterior" flexor�pronator compartment truly lies anteromedially, and the "posterior" extensor�supinator compartment lies posterolaterally. The radial artery (laterally) and the sharp, subcutaneous posterior border of the ulna (medially) are palpable options separating the anterior and posterior compartments. No motor nerves cross both demarcation, making them helpful for surgical approaches. At the level of the wrist, 9 tendons from three muscle tissue (and one nerve) of the anterior compartment of the forearm traverse the carpal tunnel; eight of the tendons share a typical synovial flexor sheath. The medial epicondyle and supra-epicondylar ridge present attachment for the forearm flexors, and the lateral formations provide attachment for the forearm extensors. Spiraling steadily over the length of the forearm, the compartments turn out to be truly anterior and posterior in position within the distal forearm and wrist.
Generic arava 10 mg with visa
These terminal branches supply the skin on the anterior aspect of the thorax and stomach treatment 4 lung cancer cheap 10 mg arava with amex. Muscular branches that offer the intercostal medicine hat weather cheap arava 20 mg without a prescription, subcostal, transversus thoracis, levatores costarum, and serratus posterior muscles. The superior half joins the brachial plexus, the nerve plexus supplying the higher limb, and the inferior half turns into the first intercostal nerve. The 1st intercostal nerve has no anterior cutaneous branch and sometimes no lateral cutaneous department. The intercostobrachial nerve often provides the floor-skin and subcutaneous tissue-of the axilla and then communicates with the medial cutaneous nerve of the arm to provide the medial and posterior surfaces of the arm. The lateral cutaneous branch of the 3rd intercostal nerve frequently gives rise to a second intercostobrachial nerve. The 7th�11th intercostal nerves, after giving rise to lateral cutaneous branches, cross the costal margin posteriorly and continue on to supply stomach skin and muscles. No longer being between ribs (intercostal), they now turn into thoraco-abdominal nerves of the anterior abdominal wall (see 761 Chapter 5, Abdomen). Their anterior cutaneous branches pierce the rectus sheath, becoming cutaneous near the median aircraft. The arterial supply to the thoracic wall derives from the thoracic aorta by way of the posterior intercostal and subcostal arteries (A, B, and D), from the axillary artery (B), and from the subclavian artery via the internal thoracic (C) and supreme intercostal arteries (B). Arterial Supply of Thoracic Wall thoracic aorta, by way of the posterior intercostal and subcostal arteries. With the exception of the tenth and eleventh intercostal areas, every intercostal house is supplied by three arteries: a big posterior intercostal artery (and its collateral branch) and a small pair of anterior intercostal arteries. The posterior intercostal arteries: of the first and 2nd intercostal spaces come up from the supreme (superior) intercostal artery, a department of the costocervical trunk of the subclavian artery. Close to the angle of the rib, the arteries enter the costal grooves, where they lie between the intercostal vein and nerve. The internal thoracic arteries (historically, the internal mammary arteries) come up in the root of the neck from the inferior surfaces of the first parts of the subclavian arteries. Between slips of the transversus thoracis muscle, the arteries contact parietal pleura posteriorly. Ipsilateral pairs of anterior intercostal arteries supply the anterior elements of the upper 9 intercostal spaces. The posterior intercostal veins anastomose with the anterior intercostal veins (tributaries of inner thoracic veins). As they strategy the vertebral column, the posterior intercostal veins obtain a posterior department, which accompanies the posterior ramus of the spinal nerve of that degree, and an intervertebral vein draining the vertebral venous plexuses associated with the vertebral column. The posterior intercostal veins of the 1st intercostal house often enter instantly into the right and left brachiocephalic veins. Although depicted right here as continuous channels, the anterior and posterior intercostal veins are separate vessels, normally draining in reverse instructions, the tributaries of which communicate (anastomose) in approximately the anterior axillary line. The left superior intercostal vein, however, usually empties into the left brachiocephalic vein. It often receives the left bronchial veins and may receive the left pericardiacophrenic vein as nicely. The recruitment of the neck muscular tissues (sternocleidomastoid, upper trapezius, and scalene muscles) is seen and notably hanging. They can also lean on their knees or on the arms of a chair to repair their pectoral girdle, so these muscles are capable of act on their rib attachments and expand the thorax. Extrapleural Access Intrathoracic Surgical Fixation makes it tough to appreciate within the embalmed cadaver, but in surgical procedure, the comparatively loose nature of the skinny endothoracic fascia supplies a pure cleavage plane, allowing the surgeon to separate the costal parietal pleura lining the lung cavity from the thoracic wall. Although primarily a sensory neuropathy (pathological change in a nerve), weak spot from motor involvement occurs in zero. Muscular weak spot usually happens in the same myotomal distribution, as do the dermatomal pain and vesicular eruptions. Vaccination confers safety in opposition to herpes zoster and is really helpful for individuals aged 60 years and older. Intercostal Nerve Block Local anesthesia of an intercostal area is produced by injecting an anesthetic agent around the intercostal nerves between the paravertebral line and the realm of required anesthesia. This procedure, an intercostal nerve block, is often used in patients with rib fractures and generally after thoracic surgery. The term block signifies that the nerve endings within the pores and skin and transmission of impulses by way of the sensory nerves carrying information about ache are interrupted (blocked) earlier than the impulses attain the spinal cord and brain. Because any particular space of pores and skin usually receives innervation from two adjoining nerves, considerable overlapping of contiguous dermatomes happens. The muscles which are really thoracic, however, present few if any surface options. The costal muscle tissue function primarily to help (provide tonus for) the intercostal areas, resisting adverse and optimistic intrathoracic pressures. Neurovasculature of thoracic wall: the pattern of distribution of neurovascular constructions to the thoracic wall reflects the construction of the thoracic cage. Breasts the breasts are the most distinguished superficial constructions within the anterior thoracic wall, particularly in ladies. The mammary glands are in the subcutaneous tissue overlying the pectoralis major and minor muscle tissue. At the greatest prominence of the breast is the nipple, surrounded by a round pigmented space of pores and skin, the areola (L. The superior two thirds of the figure demonstrates the suspensory ligaments and alveoli of the breast with resting lobules of mammary gland; the inferior part shows lactating lobules of mammary gland. They are rudimentary and functionless in males, consisting of only some small ducts or epithelial cords. The roughly round physique of the feminine breast rests on a mattress of the breast that extends transversely from the lateral border of the sternum to the midaxillary line and vertically from the 2nd via sixth ribs. Two thirds of the bed are shaped by the pectoral fascia overlying the pectoralis major and the other third by the fascia masking the serratus anterior. Between the breast and the pectoral fascia is a loose subcutaneous tissue plane or potential space-the retromammary area (bursa). This aircraft, containing a small quantity of fats, permits the breast some extent of motion on the pectoral fascia. A smaller a part of the mammary gland might lengthen alongside the inferolateral fringe of 774 the pectoralis major toward the axillary fossa (armpit), forming an axillary process or tail (of Spence). The mammary glands are firmly hooked up to the dermis of the overlying skin by substantial pores and skin ligaments (L. These condensations of fibrous connective tissue, significantly nicely developed within the superior part of the gland, help help the lobes and lobules of the mammary gland. During puberty (ages 8�15 years), the female breasts usually enlarge, owing partially to glandular improvement however primarily from increased fat deposition.
Generic arava 10 mg line
Technically symptoms of pregnancy arava 10 mg effective, nonetheless symptoms adhd arava 10 mg discount line, in every case the previous is a gross anatomy term applied to components of the grownup vertebrae, and the latter is an embryology time period referring to components of a creating vertebra ossifying from main centers. The vertebral physique is the more huge, roughly cylindrical, anterior a half of the bone that gives power to the column and helps physique weight. The measurement of the bodies will increase as the column descends, most markedly from T4 inferiorly, as every bears progressively greater physique weight. The trabecular bone is a meshwork of mostly tall vertical trabeculae intersecting with brief, horizontal trabeculae. The our bodies consist largely of trabecular (spongy) bone- 253 with tall, vertical supporting trabeculae linked by short horizontal trabeculae-covered by a comparatively thin layer of compact bone. Hyaline cartilage "end plates" cover the superior and inferior surfaces of the our bodies, surrounded by easy bony epiphysial rims. During life, a lot of the superior and inferior surfaces of the vertebral body are lined with discs of hyaline cartilage (vertebral finish plates), which are remnants of the cartilaginous model from which the bone develops. The pedicles are quick, stout cylindrical processes that project posteriorly from the vertebral physique to meet two broad, flat plates of bone, called laminae, which unite within the midline. The succession of vertebral foramina in the articulated vertebral column varieties the vertebral canal (spinal canal). Two transverse processes project posterolaterally from the junctions of the pedicles and laminae. The spinous and transverse processes provide attachment for deep again muscular tissues and serve as levers, facilitating the muscular tissues that repair or change the position of the vertebrae. Through their participation in these joints, these processes decide the types of movement permitted and restricted between the adjoining vertebrae of each region. The articular processes also help in maintaining adjoining vertebrae aligned, notably preventing one vertebra from slipping anteriorly on the vertebra under. Generally, the articular processes bear weight only temporarily, as when one rises from the flexed place, and unilaterally, when the cervical vertebrae are laterally flexed to their restrict. However, the inferior articular processes of the L5 vertebra bear weight even within the erect posture. Regional Characteristics of Vertebrae 255 Each of the 33 vertebrae is unique; nonetheless, a lot of the vertebrae show attribute options figuring out them as belonging to one of many 5 areas of the vertebral column. In addition, certain particular person vertebrae have distinguishing options; the C7 vertebra, for instance, has the longest spinous process. As vertebral column descends, our bodies improve in dimension relationship to increased weight bearing. The measurement of vertebral canal modifications in relationship to the diameter of spinal wire. The smallest of the 24 movable vertebrae, the cervical vertebrae are located between the skull and thoracic vertebrae. Their smaller size displays the fact that they bear much less weight than do the bigger inferior vertebrae. The most distinctive function of each cervical vertebra is the oval foramen transversarium (transverse foramen) in the transverse course of. The vertebral arteries and their accompanying veins cross through the transverse foramina, besides those in C7, which transmit only small accessory veins. The superior and inferior surfaces of the bodies of the cervical vertebrae are reciprocally convex and concave. Combined with the oblique orientation of the articular facets, this facilitates flexion and extension in addition to lateral flexion. The anterior arch of the atlas lies anterior to the continuous curved line fashioned by the anterior surfaces of the C2�C7 vertebral our bodies. The transverse processes of cervical vertebrae finish laterally in two projections: an anterior tubercle and a posterior tubercle. The tubercles present attachment for a laterally positioned group of cervical muscles (levator scapulae and scalenes). The inferior border of the body of the superiorly placed vertebra is reciprocally formed. The adjoining cervical vertebrae articulate in a method that permits free flexion and extension and a few lateral flexion but restricted rotation. The planar, nearly horizontal articular facets of the articular processes are also favorable for these movements. The spinous processes of the C3�C6 vertebrae are short and usually bifid in white folks, particularly males, but normally not as generally in people of African descent or in females (Duray et al. The transverse processes of the atlas arise from the lateral masses, inflicting them to be extra laterally positioned than these of the inferior vertebrae. This characteristic makes the atlas the widest of the cervical vertebrae, thus offering elevated leverage for attached muscle tissue. The occipital condyles articulate with the superior articular facets of the atlas (vertebra C1). The tooth-like dens characterizes the axis (vertebra C2) and provides a pivot around which the atlas turns and carries the skull. It articulates anteriorly with the anterior arch of the atlas ("facet for dens of the axis," partially B) and posteriorly with the transverse ligament of the atlas (see part B). Radiograph and articulated atlas and axis showing the dens projecting superiorly from the physique of the axis between the lateral masses of the atlas. The posterior arch, which corresponds to the lamina of a typical vertebra, has a large groove for the vertebral artery on its superior surface. The axis has two massive, flat bearing surfaces, the superior articular sides, on which the atlas rotates. The distinguishing function of C2 is the blunt tooth-like dens of the axis (odontoid process), which projects superiorly from its physique. The dens lies anterior to the spinal wire and serves because the pivot about which the rotation of the head occurs. This ligament extends from one lateral mass of the atlas to the other, passing between the dens and spinal wire, forming the posterior wall of the "socket" that receives the dens. Thus, it prevents posterior (horizontal) displacement of the dens and anterior displacement of the atlas. Either displacement would compromise the portion of the vertebral foramen of C1 that offers passage to the spinal wire. Thus, the first characteristic features of thoracic vertebrae are the costal sides for articulation with ribs. This arc permits rotation and a few lateral flexion of the vertebral column in this region. Attachment of the rib cage, combined with the vertical orientation of articular facets and overlapping spinous processes, limits flexion and extension in addition to lateral flexion. In radiographs of the thoracic vertebrae, the articulating ribs obscure lateral options in anteroposterior views (C) and the vertebral arch components in lateral views (D). T1 also has a whole costal aspect on the superior fringe of its physique for the 1st rib and a demifacet on its inferior edge that contributes to the articular floor for the 2nd rib. However, a lot of the transition in traits of vertebrae from the thoracic to the lumbar region occurs over the length of a single vertebra: vertebra T12. Generally, its superior half is thoracic in character, having costal sides and articular processes that allow primarily rotatory movement, whereas its inferior half is lumbar in character, devoid of costal facets and having articular processes that let solely flexion and extension.
Arava 20 mg sale
As a result medications given for bipolar disorder safe 10 mg arava, the rib might transfer superiorly symptoms 6 days before period due order arava 20 mg free shipping, overriding the rib above and causing ache. One can detect paralysis of the diaphragm radiographically by noting its paradoxical movement. Instead of ascending throughout expiration, the paralyzed dome descends in response to the constructive stress in the lungs. Structures passing between the thorax and abdomen traverse openings within the diaphragm. These embrace joints of heads of ribs and costotransverse joints, both strongly supported by a quantity of ligaments. Movements of thoracic wall: the movements of most ribs occur around a generally transverse axis that passes through the pinnacle, neck, and tubercle of the rib. Muscles of Thoracic Wall Some muscular tissues connected to and/or overlaying the thoracic cage are primarily involved in serving other areas. Axio-appendicular muscle tissue extend from the thoracic cage (axial skeleton) to bones of the higher limb (appendicular skeleton). The axio-appendicular muscles act primarily on the higher limbs (see Chapter three, Upper Limb). But several of them, including the pectoralis main and pectoralis minor and the inferior part of the serratus anterior, may also operate as accent muscles of respiration, helping elevate the ribs to increase the thoracic cavity when inspiration is deep and forceful. The scalene muscular tissues, which descend from vertebrae of the neck to the 1st and 2nd ribs, act primarily on the vertebral column. However, in addition they serve as accent respiratory muscle tissue by fixing these ribs and enabling the muscular tissues connecting the ribs beneath to be more effective in elevating the decrease ribs throughout pressured inspiration. The pectoralis major has been eliminated on the left facet to expose the pectoralis minor, subclavius, and external intercostal muscles. When the upper limb muscle tissue are removed, the superiorly tapering domed form of the thoracic cage is revealed. The true muscular tissues of the thoracic wall are the serratus posterior, levatores costarum, intercostal, subcostal, and transversus thoracis. Muscles of Thoracic Wall 749 a Action historically assigned primarily based on attachments; seem to be largely proprioceptive in operate. The role of individual intercostal muscle tissue and accent muscular tissues of respiration in moving the ribs is troublesome to interpret regardless of many electromyographic research. On the idea of its attachments and disposition, the serratus posterior inferior was stated to depress the inferior ribs, preventing them from being pulled superiorly by the diaphragm. However, it has been suggested that these muscles, which span the superior and inferior 750 thoracic apertures as well as the transitions from the relatively inflexible thoracic vertebral column to the rather more versatile cervical and lumbar segments of the column, will not be primarily motor in perform (Vilensky et al. These muscles, significantly the serratus posterior superior, have been implicated as a source of continual ache in myofascial ache syndromes. The superficial layer is formed by the exterior intercostals, the inner layer by the internal intercostals. The deepest fibers of the interior intercostals lie deep to the intercostal vessels and nerves and due to this fact are somewhat artificially designated as a separate muscle, the innermost intercostals. The exterior intercostal muscular tissues are replaced by membranes between costal cartilages. The H-shaped cuts 751 via the perichondrium of the third and 4th costal cartilages are used to shell out items of cartilage, as was accomplished with the 4th costal cartilage. The inner thoracic vessels and parasternal lymph nodes (green) lie contained in the thoracic cage lateral to the sternum. The inner thoracic arteries arise from the subclavian arteries and have paired accompanying veins (L. The continuity of the transversus thoracis muscle with the transversus abdominis muscle becomes obvious when the diaphragm is removed, as has been accomplished right here on the best side. These muscle tissue are steady inferiorly with the exterior oblique muscle tissue in the anterolateral stomach wall. Their fibers run inferoposteriorly from the flooring of the costal grooves to the superior borders of the ribs inferior to them. The inferior inner intercostal muscular tissues are steady with the inner indirect muscle tissue in the anterolateral belly wall. The inner intercostals-weaker than the external intercostal muscles-are most active throughout expiration, particularly their interosseous (vs. The innermost intercostal muscles are similar to the inner intercostals and are essentially their deeper components. These muscle tissue cross between the interior surfaces of adjoining ribs and occupy the lateralmost elements of the intercostal spaces. It is in all probability going (but undetermined) that their actions are the same as these of the interior intercostal muscular tissues. This transverse section shows nerves (right side) and arteries (left side) in relation to the intercostal muscles. The joint capsule (radiate ligament) of one costovertebral joint has been removed. Innermost intercostal muscles bridge one intercostal area; subcostal muscle tissue bridge two. Contraction of the muscle fibers that most intently parallel the slope of the ribs at a given level (fibers A and C) will elevate the ribs and sternum; contraction of muscle fibers which are approximately perpendicular to the slope of the ribs (fiber B) will depress the ribs. The subcostal muscular tissues are variable in size and form, often being nicely developed only within the decrease thoracic wall. These skinny muscular slips extend from the internal surface of the angle of 1 rib to the internal surface of the second or third rib inferior to it. The transversus thoracis muscular tissues are continuous inferiorly with the transversus abdominis muscles within the anterolateral body wall. These muscular tissues seem to have a weak expiratory perform and may provide proprioceptive info. Although the exterior and internal intercostals are energetic during inspiration and expiration, respectively, most activity is isometric (increases tonus with out producing movement); the function of those muscles in producing motion of the ribs seems to be related mainly to forced respiration. The elastic recoil of the lungs and decompression of stomach viscera expel previously inhaled air. The primary position of the intercostal muscle tissue in respiration is to support (increase the tonus or rigidity of) the intercostal space, resisting paradoxical movement especially during inspiration when internal thoracic pressures are lowest (most negative). In these circumstances, the important capacity is 755 markedly compromised by the paradoxical incursion of the thoracic wall during inspiration. Several weeks later, the paralysis turns into spastic; the thoracic wall stiffens and very important capacity rises (Standring, 2016). A pair of curved levers, representing the ribs bordering an intercostal house, are hinged posteriorly to a set vertebral column and anteriorly to a moveable sternum. The ribs (and intervening intercostal space) descend as they run anteriorly, reaching their low point roughly at the costochondral junction, and then ascend to the sternum.
Proven arava 20 mg
Continuing into the lung symptoms queasy stomach arava 10 mg discount on line, the artery descends posterolateral to the primary bronchus as the inferior lobar artery of the left lung and as an intermediate artery that may divide into middle and inferior lobar arteries of the proper lung symptoms yeast infection generic 10 mg arava overnight delivery. The arteries and bronchi are paired within the lung, branching concurrently and running parallel programs. Likewise, a paired tertiary segmental artery and bronchus supply each bronchopulmonary segment of the lung. Usually, the artery is positioned on the anterior side of the corresponding bronchus. Although the intrapulmonary relationships are precisely demonstrated, the separation of the vessels of the foundation of the lung has been 812 exaggerated within the hilar area to present them as they enter and leave the lung. Note that the right pulmonary artery passes beneath the arch of the aorta to reach the proper lung and that the left pulmonary artery lies fully to the left of the arch. Two pulmonary veins, a superior and an inferior pulmonary vein on each side, carry oxygen-rich ("arterial") blood from corresponding lobes of each lung to the left atrium of the heart. Except within the central, perihilar region of the lung, the veins from the visceral pleura and the bronchial venous circulation drain into the pulmonary veins, the relatively small volume of low-oxygen blood entering the big quantity of oxygen-rich blood returning to the center. Veins from the parietal pleura be a part of systemic veins in adjoining elements of the thoracic wall. The single proper bronchial artery may come up directly from the aorta; nonetheless, it commonly arises indirectly, either by means of the proximal part of one of the upper posterior intercostal arteries (usually the right 3rd posterior intercostal artery) or from a typical trunk with the left superior bronchial artery. The bronchial arteries supply the supporting tissues of the lungs and visceral pleura. The bronchial veins drain the more proximal capillary beds supplied by the bronchial arteries; the remainder is drained by the pulmonary veins. Then, they usually move alongside the posterior aspects of the primary bronchi, supplying them and their branches as far distally because the respiratory bronchioles. The remainder of the blood is drained by the pulmonary veins, specifically the blood coming back from the visceral pleura, the extra peripheral areas of the lung, and the distal components of the foundation of the lung. The right bronchial vein drains into the azygos vein, and the left bronchial vein drains into the accent hemi-azygos vein or the left superior intercostal vein. The superficial subpleural lymphatic plexus lies deep to the visceral pleura and drains the lung parenchyma (tissue) and visceral pleura. Lymphatic vessels from this superficial plexus drain into the bronchopulmonary lymph nodes (hilar lymph nodes) in the region of the lung hilum. The lymphatic vessels originate from superficial subpleural and deep lymphatic plexuses. All lymph from the lung leaves along the foundation of the lung and drains to the inferior or superior tracheobronchial lymph nodes. The inferior lobe of each lungs drains to the centrally positioned inferior tracheobronchial (carinal) nodes, which primarily drain to the proper facet. The different lobes of every lung drain primarily to the ipsilateral superior tracheobronchial lymph nodes. From here, the lymph traverses a variable number of paratracheal nodes and enters the bronchomediastinal trunks. The deep bronchopulmonary lymphatic plexus is positioned in the submucosa of the bronchi and within the peribronchial connective tissue. It is basically concerned with draining the buildings that type the foundation of the lung. Lymphatic vessels from this deep plexus drain initially into the intrinsic pulmonary lymph nodes, located alongside the lobar bronchi. Lymphatic vessels from these nodes continue to comply with the bronchi and pulmonary vessels to the hilum of the lung, where they also drain into the bronchopulmonary lymph nodes. From them, lymph from 816 both the superficial and deep lymphatic plexuses drains to the superior and inferior tracheobronchial lymph nodes, superior and inferior to the bifurcation of the trachea and major bronchi, respectively. The proper lung drains primarily through the consecutive sets of nodes on the right aspect, and the superior lobe of the left lung drains primarily via corresponding nodes of the left side. Many, but not all, of the lymphatics from the inferior lobe of the left lung, however, drain to the best superior tracheobronchial nodes; the lymph then continues to observe the right-side pathway. Lymph from the tracheobronchial lymph nodes passes to the right and left bronchomediastinal lymph trunks, the main lymph conduits draining the thoracic viscera. These trunks often terminate on both sides at the venous angles (junctions of the subclavian and inner jugular veins); nevertheless, the best bronchomediastinal trunk could first merge with other lymphatic trunks, converging right here to form the quick proper lymphatic duct. Lymph from the parietal pleura drains into the lymph nodes of the thoracic wall (intercostal, parasternal, mediastinal, and phrenic). A few lymphatic vessels from the cervical parietal pleura drain into the axillary lymph nodes. These nerve networks include parasympathetic, sympathetic, and visceral afferent fibers. After contributing to the posterior pulmonary plexus, the vagus nerves proceed inferiorly and turn out to be a part of the esophageal plexus, usually dropping their identity and then reforming as anterior and posterior vagal 818 trunks. Branches of the pulmonary plexuses accompany pulmonary arteries and particularly bronchi to and throughout the lungs. They synapse with parasympathetic ganglion cells (cell bodies of postsynaptic neurons) within the pulmonary plexuses and along the branches of the bronchial tree. The parasympathetic fibers are motor to the sleek muscle of the bronchial tree (bronchoconstrictor), inhibitory to the pulmonary vessels (vasodilator), and secretory to the glands of the bronchial tree (secretomotor). Their cell our bodies (sympathetic ganglion cells) are within the paravertebral sympathetic ganglia of the sympathetic trunks. The visceral afferent fibers of the pulmonary plexuses are both reflexive (conducting unconscious sensations associated with reflexes that control function) or nociceptive (conducting ache impulses generated in response to painful or injurious stimuli, such as chemical irritants, ischemia, or excessive stretch). Interalveolar connective tissue, in affiliation with Hering-Breuer reflexes (a mechanism that tends to restrict respiratory excursions). Pulmonary arteries, serving pressor receptors (receptors delicate to blood pressure). Pulmonary veins, serving chemoreceptors (receptors sensitive to blood fuel levels). The costal pleura and the peripheral part of the diaphragmatic pleura are equipped by the intercostal nerves. The anterior borders of the lungs lie adjoining to the anterior line of reflection of the parietal pleura between the 2nd and 4th costal cartilages. Here, the margin of the left pleural reflection strikes laterally after which inferiorly at the cardiac notch to reach the sixth costal cartilage. The anterior border of the left lung is extra deeply indented by its cardiac notch. On the best facet, the pleural reflection continues inferiorly from the 4th to the 6th costal cartilage, paralleled intently by the anterior border of the right lung. Both pleural reflections and anterior lung borders move laterally at the 6th costal cartilages. Thus, the parietal pleura usually extends roughly two ribs inferior to the lung. Consequently, the lungs and pleural sacs may be injured in wounds to the bottom of the neck resulting in a pneumothorax, the presence of air (G.
10 mg arava proven
The higher margins of the pubic bones (pubic crest) and the cartilaginous joint that unite them (pubic symphysis) can be felt at the inferior finish of the linea alba treatment mononucleosis buy arava 10 mg overnight delivery. The pubic crest medicine 319 arava 10 mg fast delivery, inguinal folds, and iliac crests demarcate the inferior limit of the anterior abdominal wall, distinguishing it from the perineum centrally and the lower limbs (thighs) laterally. Skin grooves additionally overlie the tendinous intersections of the rectus abdominis, which are clearly visible in individuals with well-developed rectus muscular tissues. The interdigitating bellies of the serratus anterior and exterior indirect muscular tissues are also visible. This groove is instantly visualized by having the individual drop one leg to the ground while mendacity supine on an inspecting table. The inguinal groove marks the division between the anterolateral stomach wall and the thigh. The undescended testis usually lies someplace alongside the traditional path of its prenatal descent, commonly in the inguinal canal. Because the testis wants a cooler environment for fertility as nicely, these are usually surgically corrected in childhood. Postnatal Patency of Umbilical Vein Before the delivery of a fetus, the umbilical vein carries well-oxygenated, nutrientrich blood from the placenta to the fetus. Although reference is commonly made to the "occluded" umbilical vein forming the round ligament of the liver, this vein is patent for a while after delivery and is used for umbilical vein catheterization for exchange transfusion during early infancy-for example, in infants with erythroblastosis fetalis or hemolytic disease of the neonate (Kliegman et al. This is also true of the uterus, the veins and lymph vessels of which mostly drain by way of deep routes. However, some lymphatic vessels follow the course of the round ligament via the inguinal canal. Thus, while occurring much less usually, metastatic uterine cancer cells (especially from tumors adjoining to the proximal attachment of the spherical ligament) can spread from the uterus to the labium majus (the developmental homolog of the scrotum and site of distal attachment of the spherical ligament) and from there to the superficial inguinal nodes, which obtain lymph from the pores and skin of the perineum (including the labia). These herniations occur in both sexes, however most inguinal hernias (approximately 86%) happen in males due to the passage of the spermatic twine via the inguinal canal. An inguinal hernia is a protrusion of parietal peritoneum and viscera, such as the small gut, through a standard or irregular opening from the cavity by which they belong. Most hernias are reducible, meaning they can be returned to their regular place within the peritoneal cavity by appropriate manipulation. Characteristics of direct and oblique inguinal hernias are listed and illustrated in Table B5. Normally, many of the processus vaginalis obliterates earlier than delivery, aside from the distal half that types the tunica vaginalis of the testis (see Table 5. The peritoneal a half of the hernial sac of an oblique inguinal hernia is fashioned by the persisting processus vaginalis. If the entire stalk of the processus vaginalis persists, the hernia extends into the scrotum superior to the testis, forming a whole indirect inguinal hernia (Table B5. Should a hernia be present, a sudden impulse is felt against both the tip or pad of the examining finger when the patient is asked to cough (Swartz, 2014). With the palmar surface of the finger towards the anterior belly wall, the deep inguinal ring could also be felt as a skin despair superior to the inguinal ligament, 2�4 cm superolateral to the pubic tubercle. Detection of an impulse at 1036 the superficial ring and a mass at the web site of the deep ring suggests an indirect hernia. Palpation of a direct inguinal hernia is performed by putting the palmar surface of the index and/or center finger over the inguinal triangle and asking the particular person to cough or bear down (strain). The finger can be positioned within the superficial inguinal ring; if a direct hernia is present, a sudden impulse is felt medial to the finger when the individual coughs or bears down. Cremasteric Reflex Contraction of the cremaster muscle is elicited by lightly stroking the skin on the medial aspect of the superior part of the thigh with an applicator stick or tongue depressor. This reflex is extremely energetic in youngsters; consequently, hyperactive cremasteric reflexes may simulate undescended testes. If the processus vaginalis stays patent in females, it might type a small peritoneal pouch (canal of Nuck), within the inguinal canal which will lengthen to the labium majus. In feminine infants, such remnants can enlarge and form cysts in the inguinal canal. The cysts might produce a bulge within the anterior part of the labium majus and have the potential to turn into an indirect inguinal hernia. The fluid accumulation results from secretion of an irregular quantity of serous fluid from the visceral layer of the tunica vaginalis. The measurement of the hydrocele is decided by how a lot of the processus vaginalis persists. A congenital hydrocele of the wire and testis could talk with the peritoneal cavity. Detection of a hydrocele requires transillumination, a process throughout which a bright light is utilized to the side of the scrotal enlargement in a darkened room. The transmission of sunshine as a pink glow signifies excess serous fluid in the scrotum. Newborn male infants typically have residual peritoneal fluid of their tunica vaginalis; nonetheless, this fluid is normally absorbed during the 1st yr of life. Certain pathological conditions, corresponding to injury and/or inflammation of the epididymis, may also produce a hydrocele in adults. Trauma might produce a scrotal and/or testicular hematoma (accumulation of blood, usually clotted, in any extravascular location). A hematocele of the testis may be associated with a scrotal hematocele, ensuing from effusion of blood into the scrotal tissues. Torsion of Spermatic Cord Torsion of the spermatic twine is a surgical emergency as a outcome of necrosis (pathologic death) of the testis could happen. The torsion (twisting) obstructs the venous drainage, with resultant edema and hemorrhage, and subsequent arterial obstruction. To prevent recurrence or incidence on the contralateral side, which is in all probability going, each testes are surgically fixed to the scrotal septum. Anesthetizing Scrotum Since the anterolateral floor of the scrotum is provided by the lumbar plexus (primarily L1 fibers through the ilio-inguinal nerve) and the postero-inferior side is equipped by the sacral plexus (primarily S3 fibers via the pudendal nerve), a spinal anesthetic agent have to be injected more superiorly to anesthetize the anterolateral surface of the scrotum than is critical to anesthetize its posteroinferior floor. The appendix of the testis is a vesicular remnant of the cranial finish of the paramesonephric (m�llerian) duct, the embryonic genital duct that in the feminine forms half of the uterus. The appendices of the epididymis are remnants of the cranial finish of the mesonephric (wolffian) duct, the embryonic genital duct that in the male types part of the ductus deferens. Varicocele the vine-like pampiniform plexus of veins might become dilated (varicose) and 1041 tortuous, producing a varicocele, which is usually seen solely when the man is standing or straining. The enlargement often disappears when the particular person lies down, significantly if the scrotum is elevated whereas supine, permitting gravity to empty the veins. Varicoceles could outcome from defective valves in the testicular vein, however kidney or renal vein problems can even result in distension of the pampiniform veins. Cancer of Testis and Scrotum Lymphogenous metastasis is frequent to all testicular tumors, so a knowledge of lymphatic drainage is useful in treatment (Kumar et al.
Buy arava 20 mg fast delivery
The lateral thoracic artery provides the pectoral treatment table arava 20 mg purchase without prescription, serratus anterior medicine for pink eye arava 20 mg discount, and intercostal muscular tissues, the axillary lymph nodes, and 490 the lateral aspect of the breast. The subscapular artery, the department of the axillary artery with the best diameter however shortest length, descends along the lateral border of the subscapularis on the posterior axillary wall. It quickly terminates by dividing into the circumflex scapular and thoracodorsal arteries. The circumflex humeral arteries encircle the surgical neck of the humerus, anastomosing with one another. The smaller anterior circumflex humeral artery passes laterally, deep to the coracobrachialis and biceps brachii. The larger posterior circumflex humeral artery passes medially by way of the posterior wall of the axilla by way of the quadrangular space with the axillary nerve to supply the glenohumeral joint and surrounding muscular tissues. This giant vein is fashioned by the union of the brachial vein (the accompanying veins of the brachial artery) and the basilic vein at the inferior border of the teres major. The basilic vein parallels the brachial artery to the axilla, where it merges with the accompanying veins (L. The massive variety of smaller, extremely variable veins within the axilla are also tributaries of the axillary vein. The axillary vein has three components, which correspond to the three parts of the axillary artery. Thus, the preliminary, distal finish is the third half, whereas the terminal, proximal finish is the first part. The axillary vein (first part) ends on the lateral border of the first rib, where it becomes the subclavian vein. The veins of the axilla are more abundant than the arteries, are extremely variable, and frequently anastomose. These veins constitute a collateral route that allows venous return within the presence of obstruction of the inferior vena cava (see the medical field "Collateral Routes for Abdominopelvic Venous Blood"). Axillary Lymph Nodes the fibrofatty connective tissue of the axilla (axillary fat) incorporates many lymph nodes. The axillary lymph nodes are organized in five principal groups: pectoral, subscapular, humeral, central, and apical. Of the five teams of axillary lymph nodes, most lymphatic vessels from the upper limb terminate in the humeral (lateral) and central lymph nodes. However, these accompanying the upper a half of the cephalic vein terminate within the apical lymph nodes. Lymph passing by way of the axillary nodes enters efferent lymphatic vessels that kind the subclavian lymphatic trunk, which often empties into the junctions of the inner jugular and subclavian veins (the venous angles). Occasionally, on the best side, this trunk merges with the jugular lymphatic and/or bronchomediastinal trunks to form a brief right lymphatic duct. The positions of the 5 teams of axillary nodes, relative to each other and the pyramidal axilla. The pectoral (anterior) nodes include three to five nodes that lie along the medial wall of the axilla, across the lateral thoracic vein and the inferior border of the pectoralis minor. The pectoral nodes obtain lymph mainly from the anterior thoracic wall, including many of the breast (especially the superolateral [upper outer] quadrant and subareolar plexus; see Chapter 4). The subscapular (posterior) nodes include six or seven nodes that lie along the posterior axillary fold and subscapular blood vessels. These nodes receive lymph from the posterior facet of the thoracic wall and scapular region. The humeral (lateral) nodes consist of 4 to six nodes that lie along the lateral wall of the axilla, medial and posterior to the axillary vein. These nodes receive nearly all of the lymph from the higher limb, except that carried by lymphatic vessels accompanying the cephalic vein, which primarily drain on to the apical axillary and infraclavicular nodes. There are three or 4 of those massive nodes situated deep to the pectoralis minor close to the bottom of the axilla, in affiliation with the second part of the axillary artery. Efferent vessels from the central nodes pass to the apical nodes, that are situated at the apex of the axilla alongside the medial side of the axillary vein and the primary a part of the axillary artery. The apical nodes obtain lymph from all other groups of axillary nodes in addition to from lymphatics accompanying the proximal cephalic vein. Once formed, the subclavian trunk could additionally be joined by the jugular and bronchomediastinal trunks on the right aspect to kind the proper lymphatic duct, or it might enter the proper venous angle independently. Almost all branches of the plexus arise in the axilla (after the plexus has crossed the 1st rib). This massive nerve community extends from the neck to the higher limb through the cervicoaxillary canal (bound by the clavicle, 1st rib, and superior scapula) to present innervation to the upper limb and shoulder region. The brachial plexus is usually formed by the anterior rami of the C5�C8 nerves and the larger a part of the anterior ramus of the T1 nerve (the roots of the brachial plexus). Observe the merging and continuation of certain roots of the plexus to three trunks, the separation of each trunk into anterior and posterior divisions, the union of the divisions to form three cords, and the derivation of the primary terminal branches (peripheral nerves) from the cords as the merchandise of plexus formation. Brachial Plexus and Nerves of Upper Limb 498 a Boldface (C5) signifies major component of the nerve. The roots of the plexus often move by way of the hole between the anterior and the middle scalene (L. The sympathetic fibers carried by each root of the plexus are obtained from the gray rami of the middle and inferior cervical ganglia because the roots move between the scalene muscular tissues. The anterior rami of spinal nerves C5�C8 (plus T1, concealed right here by the third a half of the subclavian artery) represent the roots of the brachial plexus. Merging and subsequent splitting of the nerve fibers conveyed by the roots type the trunks and divisions on the stage proven. The subclavian artery emerges between the center and the anterior scalene muscle tissue with the roots of the plexus. The medial and lateral pectoral nerves arise from the medial and lateral cords of the brachial plexus, respectively (or from the anterior divisions of the trunks that type them, as shown right here for the lateral pectoral nerve). The courses of the median and musculocutaneous nerves and the standard sample of branching of their motor branches are shown. The course of the ulnar nerve and the standard sample of branching of its motor branches. The courses of the axillary and radial nerves and the typical pattern of branching of their motor branches. The posterior 502 interosseous nerve is the continuation of the deep branch of the radial nerve, shown right here bifurcating into two branches to provide all of the muscular tissues with fleshy bellies positioned entirely in the posterior compartment of the forearm. The dorsum of the hand has no fleshy muscle fibers; subsequently, no motor nerves are distributed there. Anterior divisions of the trunks provide anterior (flexor) compartments of the upper limb, and posterior divisions of the trunks supply posterior (extensor) compartments.